Avalere analysis shows mixed results for federal value-based payment models
Despite the poor financial results to-date, the Trump administration was not expected to fundamentally rethink value-based payment.
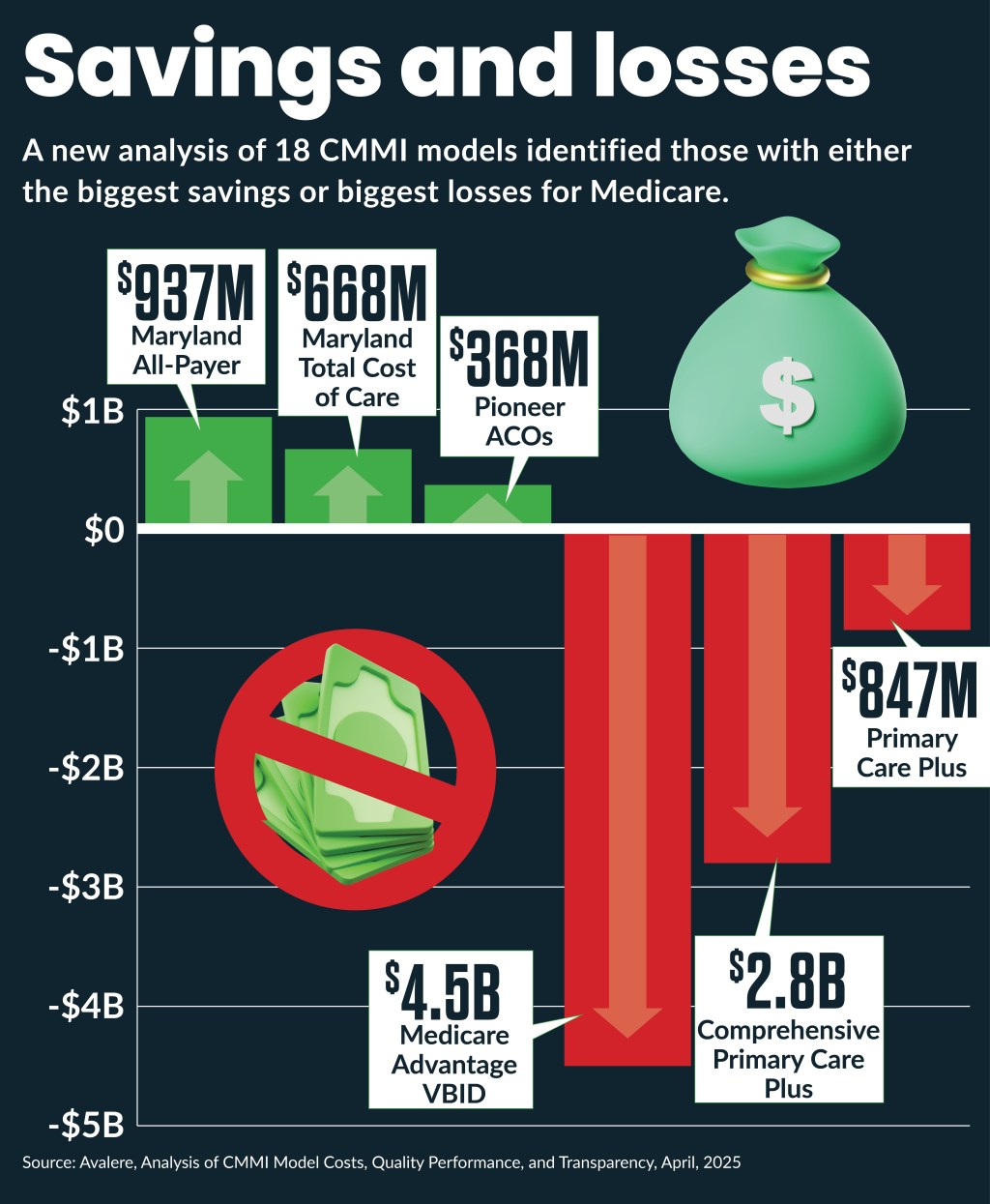
Eighteen value-based payment models implemented by the federal government drove a net increase of $7.7 billion in federal spending, according to recent analysis.
Avalere’s report examined 18 models implemented by the CMS Center for Medicare and Medicaid Innovation (CMMI), 15 of which were later expanded and a few discontinued, and found some provided $2.6 billion in Medicare savings while others increased Medicare spending by $10.3 billion.
The widely disparate results of the models generally fell in three categories:
- One-third yielded substantial net Medicare savings
- One-third generated substantial net Medicare losses
- One-third had nominal financial impacts
The net results included administrative costs to Medicare but did not account for often-substantial provider costs to participate in the models.
Since its launch, CMMI has implemented and evaluated over 50 models, and the HHS has selected four for nationwide expansion.
Significance seen
The findings did not surprise Guy D’Andrea, executive director of the Catalyst for Payment Reform.
“There have been other studies that the CMMI models had a mixed set of results; some of them showing more promise than others,” D’Andrea said. “The fact that some of these models show promise and some don’t is the way that the process is supposed to work.”
The models with the largest Medicare net savings included:
- Maryland All-Payer, $937 million
- Maryland Total Cost of Care, $668 million
- Pioneer ACOs, $368 million
Models with the largest net costs to Medicare included:
- Medicare Advantage VBID, $4.5 billion
- Comprehensive Primary Care Plus, $2.8 billion
- Primary Care First, $847 million
Policy effects
The report comes amid a Trump administration shakeup of CMMI models. In March, CMMI announced plans to terminate four active models and cancel the development of two proposed models to focus on models for expansion based on projected savings and quality outcomes.
“I don’t think there will be a major shift as a result of this report,” D’Andrea said.
However, policy changes he did expect from the Trump administration for CMMI models include:
- More all-payer models
- More two-sided risk models
- More mandatory models
- Increased transparency
The all-payer model push could be accelerated by the report’s findings that such models provided the biggest savings.
Such results also demonstrated the potential for commercial payers to undertake accelerated shifts to value-based payment.
Little in the report focused on the role of downside risk in CMMI models but D’Andrea noted reports that have found downside risk is continuing the increase among all payer categories. Many providers have raised concerns about downside risk if organizations lack the infrastructure or financial stability to take on risk.
But D’Andrea was optimistic such capabilities would increase as payers increase their adoption of it.
“There are always going to be technical and market-based challenges in the adoption of these programs but, so far, the industry has demonstrated an ability to solve them,” D’Andrea said.
Mandatory questions
The Avalere report found mandatory models may only generate nominal financial savings without significant quality improvements. It cited results for the ESRD Treatment Choices (ETC) Model ($86 million in Medicare losses over six years) and the Comprehensive Care for Joint Replacement (CJR) model ($29 million in Medicare losses over eight years).
However, the findings on mandatory models likely won’t affect policymakers’ preference to push more mandatory models to drive more industry change and generate more savings, D’Andrea said.
“Ultimately, voluntary programs are still subject to the self-selection influence that undermines their results,” D’Andrea said. “When we think about the broader marketplace, we would like to see engagement in value-based care delivery as a market requirement. To be a successful provider system, you should be focused on delivering optimal care quality, managing population health, limiting costs.”
Transparency need
The Avalere report found many CMMI models did not publicly report financial or quality data from the models, which could hinder the ability of providers to learn from their results.
“There should be a goal to share as much of the evaluation results as possible,” D’Andrea said.
Increased transparency also could help commercial payers to learn from CMMI models results, he said.
The Avalere report found CMMI efforts to gather public input on the models were limited to only nine models soliciting comments on model development or refinement through rulemaking or requests for information. But D’Andrea said that may have failed to account for informal CMMI stakeholder engagement initiatives on design elements.
“They could probably do more to ensure there are numerous ways to gather public input on the design,” D’Andrea said. “But I don’t think it would be accurate to say they haven’t considered public input in the past.”
Foundational questions
The findings may fuel criticisms that CMMI and even value-based approaches need to be fundamentally rethought.
CMMI draw criticism from congressional Republicans at a 2024 hearing based on the 2023 CBO findings that it was not on track to provide the $80 billion in 20-year savings estimated by the CBO when the office was created under the Affordable Care Act. Instead, it increased costs by $5.4 billion in its first decade and was projected to increase spending by over a billion dollars in the second decade.
“[W]hen the administration changed in 2017, and I immediately thought here is our chance to remove CMMI, the Congressional Budget Office said you can’t do that because of all these savings that are built into the law,” said Rep. Michael Burgess (R-Texas). “But then it turns out those savings were ephemeral, and they weren’t really savings at all, were they?”
Some conservative policy groups have recently called for the elimination of CMMI.
But the ability of some models to produce savings could ensure CMMI’s future.
“I’m confident that the programs will continue to produce long-term savings, especially as they focus more on those programs that demonstrably have generated savings,” D’Andrea said.





