Florida hospitals face scrutiny for transparency practices
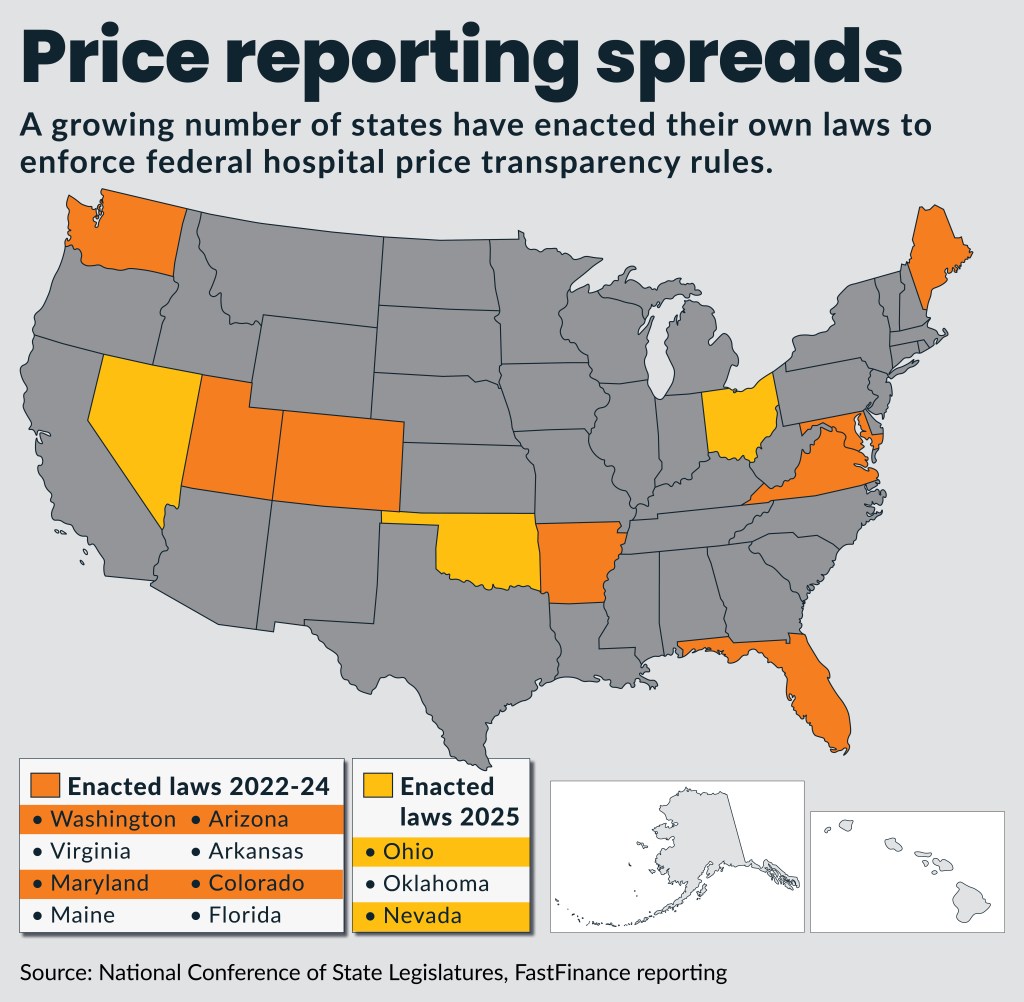
States are increasingly looking to take on enforcement of hospital price transparency.
Florida has launched a unique hospital price transparency criminal enforcement initiative, as a growing number of states enact their own transparency laws with civil penalties.
On May 30, Florida Attorney General James Uthmeier announced he was investigating Florida hospitals over their price transparency and billing practices. Florida is one of a growing number of states that have enacted its own price transparency law for hospitals since federal rules were first announced in 2019.
The probe includes subpoenas to multiple hospitals to gather more information about their transparency practices and billing processes. Uthmeier said his actions aim to enforce state law barring unfair and deceptive acts and practices, including the omission of material information like prices. The action appears to fall under antitrust criminal law in the state and not a civil statute, according to a knowledgeable source in the state. The attorney general’s office did not respond to requests for clarification.
Florida enacted a law in 2024 that echoed provisions of federal price reporting requirements, but the attorney general’s action differs from civil enforcement provisions in that law.
“For years, many hospitals have extorted patients who’ve come in with life-or-death cases and left with crippling debt,” Uthmeier said.
The subpoenas to at least two health systems in the state have raised concerns among Florida hospital executives.
“Certainly, we are concerned about the perception that this enforcement action creates, especially some of the commentary from the attorney general related to his social media posts and the use of subpoenas when hospitals have been absolutely committed to pricing transparency, the new federal requirements and long committed to all of the efforts in Florida to provide meaningful pricing information to consumers,” said Mary Mayhew, president and CEO of the Florida Hospital Association (FHA).
Hospitals had not heard any indication that such an enforcement action was under consideration, Mayhew said. Hospitals have not heard what the attorney general plans to do with the subpoenaed information.
“Those health systems are focused on full cooperation with the attorney general’s office and a continued commitment to publicly accessible, meaningful consumer information,” she said.
Federal role
Uthmeier also said his enforcement initiative was inspired by President Donald Trump’s Feb. 25 executive order demanding greater hospital price transparency. That order directed federal regulators to issue new rules within 90 days to require, in part, “the disclosure of the actual prices of items and services, not estimates.”
On May 22, CMS’s updated price transparency instructions to change machine-readable files (MRFs) to place more responsibility on hospitals to provide the dollar amounts they charge for services. In conjunction with the guidance, CMS sent out a request for information (RFI) on ways to promote hospital compliance with accuracy and completeness standards regarding price transparency.
Since 2022, 27 hospitals have been fined varying amounts by CMS for falling short of price transparency regulations, according to the agency’s data.
Mayhew said some regulatory approaches may be counterproductive because they don’t help most patients, who are insured and need to know their out-of-pocket costs for various services.
State laws
Seven states (Washington, Virginia, Maryland, Maine, Arizona, Arkansas and Colorado) implemented laws echoing federal transparency requirements from 2022 to 2024, according to tracking by the Nation Conference of State Legislatures. So far this year, three more states (Ohio, Oklahoma and Nevada) also enacted price transparency laws for hospitals tied to federal rules.
The state transparency laws usually seek to codify federal transparency regulations under state law, but some add their own enforcement provisions or expand the reporting requirements to additional types of providers.
Some state laws are driven by reports that large numbers of hospitals in the state were out of compliance with the federal rules, said Stacey Pogue, a senior research fellow at the Center on Health Insurance Reforms (CHIR) at Georgetown University’s McCourt School of Public Policy.
“Those messages were getting back to the statehouses, that compliance wasn’t at 100% for something voters were pretty excited about,” Pogue said.
Ohio’s law, implemented April 3, echoes federal transparency rules plus, requires hospitals to provide the state Department of Health with annual updates on their price lists or price tool. Additionally, the state will publicly post which hospitals are non-compliant, issue state penalties (in amounts determined by an administrator) for non-compliance and bar some hospital uses of personal information collected from those seeking price information.
Oklahoma’s law, enacted May 27, mirrors federal requirements, plus non-compliant hospitals cannot undertake debt collection for any service where prices were not listed, as required. Additionally, non-compliant hospitals must refund any payer what they have paid and pay a penalty to the state in that amount, dismiss any court action and pay attorney fees, and remove any credit agency reporting related to the debt.
Nevada’s law, enacted June 6, also mirrors federal rules. Additional provisions include:
- Barring non-compliant hospitals from collecting medical debt or referring debt to collection agencies
- Requiring hospitals to provide patients with itemized statements and receipts before attempting to collect medical debt
- Canceling medical debt if hospitals fail to provide advance information
- Authorizing penalties from $600 to $11,000, based on the hospital’s size
- Authorizing the governor’s Consumer Health Advocate to help patients file claims against healthcare entities that violate requirements
The approach of Oklahoma in barring debt collection actions and issuing fines to mirror debt amounts sought by non-compliant hospitals may be a way states are seeking to enforce their laws without adding regulatory enforcement costs to the state, Pogue said.





