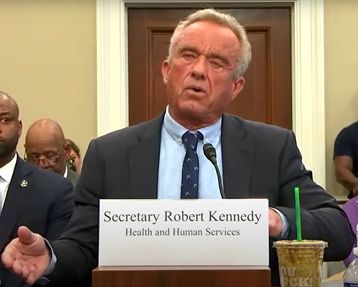
RFK Jr. defends HHS budget to Congress and talks Medicaid, 340B and more
The HHS secretary said his department’s hands are tied regarding a specific financing boost for rural hospitals.
In congressional testimony, HHS Secretary Robert F. Kennedy Jr. endorsed proposed Medicaid cuts as affecting fraud, waste and abuse rather than beneficiaries who most need the program.
Speaking May 14 before a House Appropriations subcommittee and later the Senate Health, Education, Labor and Pensions (HELP) Committee, Kennedy also indicated a willingness to pare down the 340B Drug Pricing Program and addressed the challenges facing rural hospitals.
The official reason for Kennedy’s appearance on Capitol Hill was to discuss the Trump administration’s proposed HHS budget and the department’s restructuring plans for FY26. Relative to FY25, the funding cut would be 26%.
The budget request “includes reforms to put healthcare spending on a sustainable fiscal path,” Kennedy said.
He touted workforce reductions that have eliminated roughly 20,000 of 82,000 positions, for savings of $1.8 billion per year. The restructuring plan will consolidate the department’s 28 divisions into 15, but Kennedy said developments in ongoing litigation prevented him from giving details on the fate of specific programs.
Kennedy’s strategy to address chronic illness via initiatives focused on the nation’s food and water supply and environmental toxins “will be reflected in the reorganization,” he said, while the reductions also are meant to improve HHS’s efficiency and responsiveness without impairing oversight of Medicare, Medicaid and other essential health services.
Democrats also sought to press Kennedy on attempted claw-backs of FY25 appropriated funding, including a reported $11.4 billion in public health grants for states and municipalities and $2.7 billion in National Institutes of Health funding.
“That is contrary to the money appropriated,” said Rep. Rosa DeLauro (D-Conn.).
Kennedy did not substantively respond to the allegation.
“If Congress appropriates to me the money, I’m going to spend the money,” he said.
Medicaid cutbacks
Three days after House Republicans released proposed legislation that includes a $715 billion cut in projected 10-year federal healthcare spending, mostly in Medicaid, Kennedy supported the GOP position that the cuts would not affect the traditional classes of Medicaid beneficiaries. In related news Wednesday, the Energy and Commerce Committee voted along party lines to advance the healthcare portion of the bill to the full House for consideration.
“The cuts to Medicaid are for fraud, waste and abuse,” Kennedy said in response to a question. “Because of DOGE, we were able to determine that a million people are claiming Medicaid from multiple states. That’s illegal, it’s theft, you’re not allowed to do that.”
He also said the cuts would remove coverage for more than 1 million illegal immigrants, while another category that would be affected “is adults who are able-bodied, who refuse to look for a job [or] to volunteer.”
The Congressional Budget Office’s updated projections for the reconciliation bill suggest 10.3 million people would lose Medicaid coverage over 10 years.
Of that total, 1.6 million would be disenrolled from coverage in a second state but would retain coverage in their state of residence. In addition, 1.3 million dual-eligibles would retain Medicare coverage but would lose access to the cost-sharing support and long-term-care coverage available through Medicaid. An estimated 1.4 million would lose coverage due to unverified citizenship, nationality or satisfactory immigration status.
After accounting for those groups, roughly 6 million additional beneficiaries would lose Medicaid. The CBO’s numbers do not specify the impact of each policy, but in addition to a work requirement beginning in 2029, provisions in the reconciliation bill would repeal Biden administration regulations designed to streamline eligibility verification, enrollment and renewal processes and would require more frequent eligibility checks for expansion enrollees.
Concerns about unintended consequences
With respect to the work requirement, one reason for trepidation among critics is that the policy could strip people of coverage due to administrative snags rather than chronic unemployment. A study released May 13 by the left-leaning Center on Budget and Policy Priorities posited that at least 9.7 million people would lose Medicaid by 2034 as a result of the proposed policy.
The number would be higher if states implement the policy stringently and fail to effectively use data matching to exempt beneficiaries from the requirement. At least two-thirds of those losing coverage either would be employed or eligible for an exemption (e.g., due to disability, school attendance), according to the study.
“We’ve seen it time after time, including in Arkansas and Florida and other states, that when you put more red tape in front of people actually getting that lifesaving care, you’re going to prevent people from accessing health insurance,” Rep. Josh Harder (D-Calif.) said during the House hearing (Florida has not implemented a Medicaid work requirement; to date, only Arkansas and Georgia have done so).
To Kennedy, the program has become bloated.
“Medicaid is for poor children, it is for women — for mothers — and it’s for the disabled,” the secretary responded.
340B changes loom
One question that came up during the House hearing concerned the proposed shift of the 340B program from the Health Resources and Services Administration (HRSA) to CMS. HRSA would cease to exist as a stand-alone agency, with core operations moving over to a newly created Administration for a Healthy America.
Kennedy said he could not comment on the shift in 340B oversight, citing the advice of attorneys amid ongoing litigation about the HHS restructuring. But he indicated his feeling that the program has exceeded its intent.
“It’s not a straightforward program because it was originally intended for a hundred institutions that were serving very poor communities. It’s now grown to 27,000 institutions,” Kennedy said (the number of hospitals participating in January 2023 was 2,600, according to the Government Accountability Office). “The patients themselves seldom get the benefits of the drug [price] reduction.
“But we also recognize that it is the lifeblood of rural hospitals right now, so we can’t mess with that program without giving those rural hospitals something else that is going to support them.”
Rep. Chuck Fleischmann (R-Tenn.) referred to President Donald Trump’s recent executive order that aims to reduce drug costs by linking prices to those in comparable nations. The congressman seemed to imply 340B policy should be reconsidered in conjunction.
By lowering the price of all drugs, the policy “will further lower the cost of 340B drugs,” Fleischmann said. “And [drug manufacturers] consider that existential, so this is a problem we all need to work out together.”
Attention on rural hospitals
Kennedy took a question about the Medicare area wage index, which affects the ability of rural hospitals to pay competitive wages.
“By keeping these hospitals at the lower end of the wage spectrum, they cannot compete against higher-paying hospitals, increasing their risk of closure and locking them into a downward spiral,” said Rep. Robert Aderholt (R-Ala.), chair of the subcommittee that held Wednesday morning’s hearing.
He noted that Trump’s first administration implemented a supplemental payment for hospitals toward the bottom of the wage index. But other hospitals challenged the policy in court, saying it unlawfully reduced their payments due to budget neutrality requirements, and the plaintiffs secured vacatur of the policy in a 2024 ruling. CMS subsequently terminated the policy going into FY25.
Said Kennedy, “We got a very bad decision from that [court ruling] that said my agency has no power to redress this disparity. I pledge to work with you and with Congress. The change has to be statutory, and we will do our job providing technical support, including the kind of studies that show how badly this disparity is wounding rural America.”
He also said workforce programs will continue to bolster clinical staffing at rural providers and that hospitals will be supported as needed. He promoted telehealth as a way to improve healthcare access for rural communities, giving the example of technology that allows for a strep throat diagnosis based on a single image taken with the patient’s phone.
“We are going to dramatically revolutionize the availability of telehealth and AI so that people can avoid emergency rooms by getting treated at home,” he said.





