Providers, payers both struggle with Medicare Advantage challenges
As seen in reporting from the two sectors, the MA program presents an array of stumbling blocks to optimal financial performance.
Note: This article was updated May 13 where noted.
Neither providers nor a leading payer are finding much reason for satisfaction with the state of Medicare Advantage (MA) these days.
Q1 financial reporting by for-profit hospital chains and by UnitedHealth Group (UHG), among other payers, have reflected the challenging landscape.
UHG in April shared what the company’s leaders described as disappointing financials, and the key driver was an unanticipated rise in physician and outpatient care activity among UnitedHealthcare’s MA members.
Such trends arguably bode well for population health but not for an insurer’s bottom line.
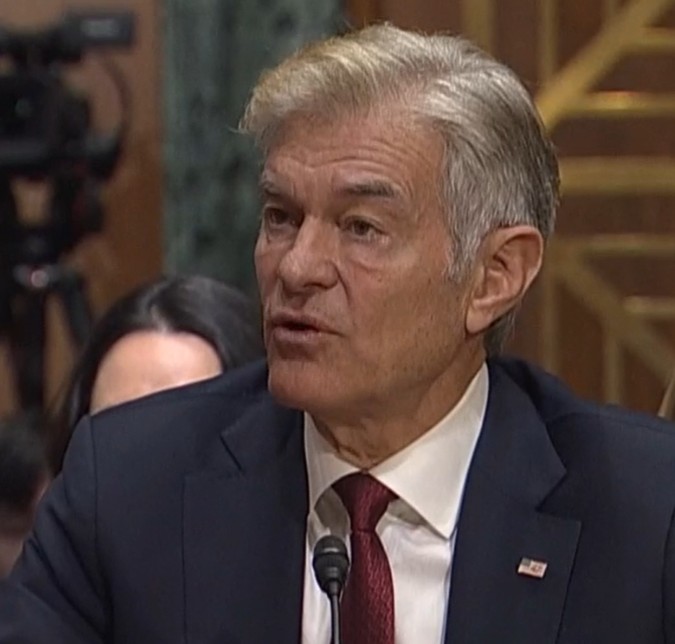
“We had planned for 2025 care activity to increase at a rate consistent with the utilization trend we saw in 2024,” said UHG CEO Andrew Witty. “Instead, first-quarter 2025 indications suggest care activity increased at twice that rate.” (May 13 update: Witty has stepped down as UHG’s CEO and has been replaced by Stephen Hemsley, who was the company’s CEO from 2006 until 2017 and will retain his current position as board chair, the company announced).
Flu activity was higher than average, but UHG leaders seemed to be referencing increases in elective care.
Company leaders partially attributed the utilization spike to higher premiums in the public-sector group MA space, with the premium increase having stemmed from greater Medicare spending. The theory goes that when members pay more for premiums, they are more likely to seek care as a way to get their money’s worth.
“Another example across senior populations was the earlier and higher wellness-visit activity we saw, which drives specialty and outpatient utilization,” said John Rex, UHG’s CFO.
Factors that had been mentioned as accelerating the company’s MA costs in 2024 included provider upcoding and costs of specialty drugs. But Tim Noel, who was named CEO of UnitedHealthcare in January, said those issues have been in line with 2025 projections and thus are not spurring the company’s higher-than-expected costs.
Meanwhile, insurers such as Humana, CVS Health and Centene recently have described strategies to reduce their MA footprint as they seek to scale back on unprofitable plans.
Reading the tea leaves
Medicare Advantage policymaking and regulatory activity suggest a mixed bag for insurers moving forward.
The Trump administration issued an MA payment increase that was higher than expected for 2026, at 5.06% ($25 billion) before factoring in the boost from risk-score trends. The proposed increase issued by the Biden administration had been 2.23%. CMS says the difference primarily stems from an update to Medicare spending data.
At the same time, Dr. Mehmet Oz, CMS administrator, is among the officials who have said they see a need to go after MA plans for upcoding practices. Such an effort would have the support of congressional Democrats, some of whom recently drafted a letter to congressional Republican leadership to suggest that a crackdown on upcoding should take precedence over Medicaid spending cuts in the ongoing budget reconciliation process.
Compared with enacting potentially deep Medicaid cuts, according to the letter, going after MA upcoding would be a more viable way to tackle fraud, waste and abuse in healthcare.
The Trump administration’s Department of Justice also recently announced it would pursue a False Claims Act complaint against Aetna (CVS Health), Elevance and Humana, along with three insurance brokers, in response to an alleged scheme that involved hundreds of millions of dollars in kickbacks to the brokers for MA enrollment initiatives. The three plans and the brokers all responded that they did not engage in misconduct or illegal activity.
Even amid a willingness to challenge MA plans in aspects such as upcoding and marketing, the push to streamline the federal bureaucracy suggests the administration could be amenable to shifting more of the Medicare apparatus to the private sector (i.e., MA) via regulations and payment models. Oz himself has previously advocated for a Medicare Advantage for All system.
Provider concerns
Providers long have reported difficulty with denials and downgrades across payer segments, but recent years have shined a spotlight on the issue particularly in Medicare Advantage.
Challenges in getting hospital visits classified as inpatient admissions are seen at many providers, including HCA Healthcare, where MA observation rates remain roughly 15% higher than those in traditional Medicare, according to Q1 reporting.
Mike Marks, the company’s CFO, said that despite 2023 guidance from the Biden administration on applying two-midnight standards in MA, “We really did not see any additional movement from observation to inpatient status related to the adoption of the two-midnight rule.”
In a wide-ranging report on the healthcare costs incurred by hospitals, the American Hospital Association said observation stays were 28.6% longer in MA than in traditional Medicare in 2019. By 2024, the gap had risen to 36.9%.
Another area of inefficiency in MA, according to the AHA’s report, is in discharges from hospitals to post-acute care facilities. Hospital stays leading up to such discharges were 6.4% longer in MA than in traditional Medicare in 2019, and the difference increased to 12.6% in 2024. Hindrances include prior authorization requirements and inadequate post-acute provider networks.
Negotiated MA payment rates also are lower than in traditional Medicare, sometimes by several percentage points, according to the report. Administrative complexity in the program is also increasing, especially in the form of required prior authorizations, which totaled nearly 50 million in 2023 and had risen by more than 40% over the prior three years.
Such trends may induce providers to transfer their MA participation from PPOs to HMOs, according to an HFMA analysis written by Providence COO Deepak Sadagopan. And some smaller hospitals have been choosing to exit the program altogether.





