Hospital ED volumes hike 40% since 2020, according to Moody’s report
The recent 40% increase is much faster than 20% increase that occurred in the two decades preceding the pandemic.
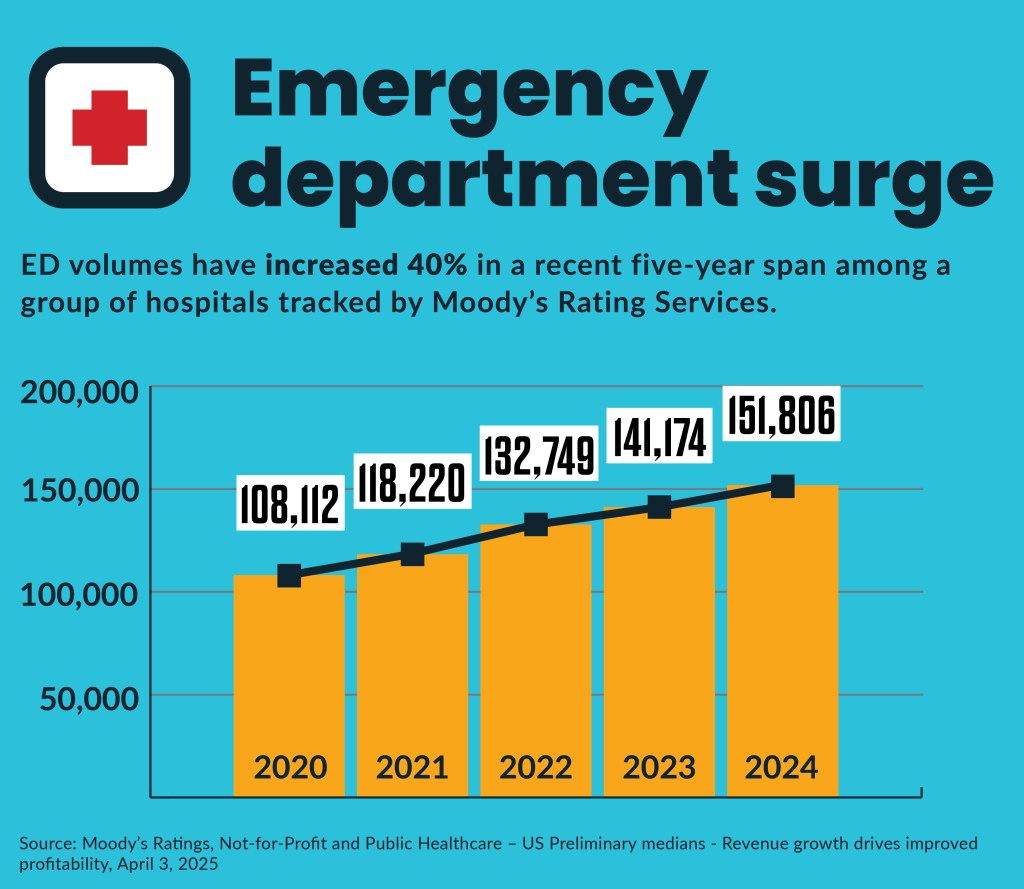
Hospital emergency department (ED) volumes have jumped 40% since 2020, according to a recent rating agency report.
Annual total ED volumes increased among the 123 hospitals rated by Moody’s from 108,000 in 2020 to nearly 152,000 in 2024, according to a recent report (subscription required). After an 8% decrease in volumes in 2020 during the peak of COVID-19 concerns, ED volumes surpassed 2019 pre-pandemic volumes by 2023, a Moody’s report last year of a separate group of 215 hospitals found.
The data echoed other reports and ED volume concerns raised by various hospitals in recent years. For example, the latest Kaufman Hall hospital flash report found year-to-date ED visits per calendar day increased 15% compared to 2022 among the more than 800 hospitals it tracked.
It was a faster increase than seen in the years before the COVID-19 pandemic, when ED volumes increased 20% from 2000 to 2018, according to data from the Centers for Disease Control and Prevention (CDC).
“We have seen an increase in the last few years,” said Nicholas Mohr, MD, professor of Emergency Medicine, Anesthesia Critical Care, and Epidemiology at the University of Iowa Carver College of Medicine.
Health drivers
However, Mohr views the recent increase as just the latest leg in an ongoing trend of greater ED utilization over several decades and not a crisis. That’s because it is driven by an increasingly sick population seeking high-acuity care — including labs, imaging and specialists — together in one convenient location, he said.
“Most emergency department utilization is not for uninsured people who don’t have other places to go,” Mohr said. “Most of it is for people who have serious medical conditions.”
More, sicker ED patients seen in the ED are increasing the share of ED patients admitted to the hospitals, he said.
CDC data on ED visits in 2021 compared to 2019 found:
- 13.1% versus 11.2% were admitted
- 2.3% versus 2.6% were admitted for observation
- 1.6% versus 1.7% were transferred to another hospital
Higher admissions rates were especially seen among larger regional hospitals, according to previous research.
“It’s a function probably of more technology and the ability to intervene on more diseases,” Mohr said. “Hospitals that have the most capabilities tend to also be the places that are the most crowded.”
Payer role
The ED surge is unlikely tied to the popular conception that EDs are flooded by uninsured people seeking care, since it is the only healthcare location required by law to treat patients regardless of their ability to pay, he said.
“It’s really a minority of care that is being delivered,” Mohr said about uninsured volumes in EDs.
The share of uninsured ED volumes has decreased since the Affordable Care Act’s (ACA) coverage expansions went into effect in 2013 — dropping from 19.1% in 2013 to 9% in 2021, according to CDC data. However, due to the ACA’s Medicaid coverage expansion, Medicaid ED volumes increased from 32.1% in 2013 to 45.3% in 2021. Medicaid enrollees have comprised the largest share of ED patients since mid-2013, according to the data.
However, some states and hospitals have reported ED volume surges by uninsured patients, which they blamed on the nearly 11 million-person surge in illegal immigrants since 2021 and the post-COVID restart of Medicaid eligibility determinations. For example, Colorado reported that uninsured ED visits increase from 6.6% in mid-2023 to 9.8% in October 2024.
“It highlights the impact of both the migrant surge, which began in December 2022, as well as the Medicaid PHE [Public Health Emergency] unwind on uninsured hospital ER visit rates,” Lisa Rothgery, chief medical officer for the Colorado Cost Control and Quality Department, said in a presentation on state hospital data.
The Medicaid redeterminations occurred from May 2023 to April of 2024.
The percentage of adults living in the United States who were uninsured did not significantly change between 2023 (10.9%) and the first six months of 2024 (11.1%), according to a December 2024 CDC report.
The ED surge comes despite an industry-wide and federal regulatory push to divert patients with low-acuity conditions, as well as preventing health deteriorations of treated and discharged patients from seeking care in the ED. For example, many CMS value-based payment models include reduced ED usage as a primary endpoint.
Mohr agreed that healthcare organizations have greatly increased the number of low-acuity sites.
“In many cases, that’s where people who have low-acuity conditions are going,” he said.
However, EDs are increasingly crowded “because people have high-acuity problems that need to be seen in emergency departments,” Mohr said. “We know our population’s aging; the medical problems that are bringing people to the hospital have been increasing. This has become the predominant way that people who have conditions that require hospitalization come into the healthcare system.”





