Fraud and waste in Medicaid: Congressional panel calls for legislative action
Proposed changes mostly focused on improving Medicaid eligibility determinations.
The first hearing of Congress’ new government efficiency panel featured a large focus on needed changes to Medicaid.
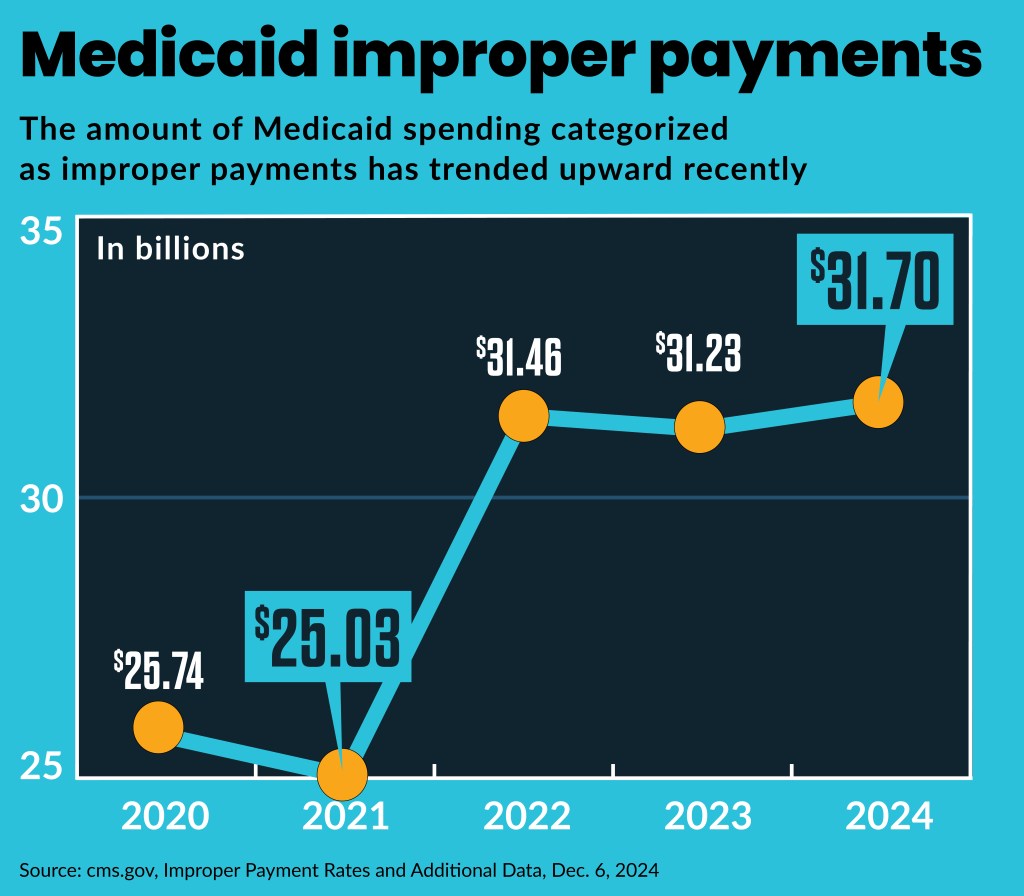
The newly created House Oversight Delivering on Government Efficiency (DOGE) Subcommittee held a hearing Feb. 12 on the $236 billion in 2023 federal improper payments, including fraud, and featured testimony from several witnesses long-experienced in leading anti-fraud efforts.
“Unfortunately, as Medicaid has grown, so too has its mismanagement,” Stewart Whitson, senior director of federal affairs at the Foundation for Government Accountability, said to the panel. “Nearly one-third of all federal improper payments are attributable to Medicaid.”
Similarly, Dawn Royal, director of the United Council on Welfare Fraud, highlighted billing fraud in Medicaid from providers submitting claims for services never rendered or overcharging for services. She cited a Government Accountability Office report that found Medicare and Medicaid paid a combined total of over $100 billion in improper payments in 2023.
“I’m looking to what we find out and how we solve this crisis,” said Rep. Marjorie Taylor Greene (R-Ga.), chair of the panel.
Democrats said they also were interested in reducing improper payments but that the effort was undermined by the parallel efforts of the White House’s newly created DOGE, led by Elon Musk.
“While we’re sitting here, Elon Musk and Donald Trump are recklessly and illegally dismantling the federal government,” said Rep. Melanie Stansbury (D-N.M.), a ranking member of the panel.
Greene said in a podcast interview that same week that the new congressional panel will aim to provide the legislation needed to stop and prevent any fraud waste and abuse identified by the DOGE administrative effort.

Recommendations
The witnesses told the panel that federal legislation is needed to prevent healthcare fraud and waste that they have found, and the fraud is increasingly driven by foreign criminal organizations.
Haywood Talcove, CEO of LexisNexis Risk Solutions, said criminals are using AI to “supercharge” fraud, which has produced a 20% fraud rate in public programs, while the private sector has a 3% fraud rate.
A key changed needed in federal healthcare programs is implementation of identity verification at enrollment, elimination of self-certification and ongoing auditing. The current under-funded anti-fraud apparatus and enrollment systems instead leave federal programs to chase criminals after they are paid.
“Pay and chase does not work,” he said.
Talcove said needed legislative changes include:
- Updating the 1974 federal privacy law to allow data sharing and matching
- Including anti-fraud funding in each appropriation bill
- Barring permanently and heavily fining those who steal from entitlement programs
- Eliminating broad-based categorical eligibility
Needed administrative changes, said Royal, included reversing provisions of a Biden administration Medicaid rule, which barred states from recovering the cost of Medicaid services from a beneficiary, even after they were criminally convicted. Whitson said reversing the rule would provide $164 billion in federal savings over 10 years.
Other provisions in the rule that were fueling fraud and improper payments, he said included:
- Barring states from verifying eligibility more than once a year
- Prohibiting in-person or phone interviews to verify the identity of the applicant
- Opening a lengthy reconsideration period — 90 days — which allows undocumented immigrants to get Medicaid benefits
Bureaucratic opposition
The Trump administration has drawn criticism from Democrats and unions for firing federal bureaucrats, including a reported 5,200 civil servants from the Department of Health and Human Services.
However, witnesses told the panel that federal bureaucrats have frequently created obstacles to their past fraud fighting efforts.
“Sadly, it is already apparent that career bureaucrats are not being totally transparent as they attempt to protect spending or broken programs,” Royal said. “We fail to understand how failing to mitigate the rampant fraud in Medicaid, SNAP, and other welfare programs stand up or strengthens the welfare programs.”
An example cited was the Department of Agriculture’s delay in implementing a National Accuracy Clearinghouse (NAC), despite congressional mandates for nationwide implementation. Talcove said a NAC pilot program already identified more than 14 million cases of duplicate participation in Medicaid, SNAP and Temporary Assistance for Needy Families (TANF), and prevented billions of dollars in improper payments.
Republicans highlighted previous efforts by Democratic presidents to improve the federal government’s efficiency through workforce reductions. For example, President Bill Clinton announced he would implement savings recommended to him by cutting 12% of federal workforce. He ultimately eliminated 377,000 federal positions between 1993 and 1999.
Medicaid eligibility
Whitson said 80% of Medicaid improper payments are due to eligibility errors.
“If Congress wants to help President Trump target wasteful spending, then targeting eligibility errors in Medicaid should be one of your top priorities,” Whitson said.
Royal said states are hesitant to spend their own funds to protect federal dollars through anti-fraud efforts. That is because, in many states, the federal government provides three-quarters of the Medicaid funding, so states would only recoup 25% from any anti-fraud efforts.
Some states are using private sector technology to improve eligibility determinations over systems relied on by the federal government, said witnesses. For example, Missouri is now rolling out statewide, a private company program, called SteadyIQ, to verify income for Medicaid, food assistance programs and temporary assistance for needy families. The state piloted the program, which can verify regular income and so-called gig income — like food delivery work — for applicants to its public programs.
“All we have to do is adopt what has already been proven in Missouri and we’ll save 20%,” said Rep. William Timmons (R-S.C.). Such a program, if adopted nationwide, would save almost $200 billion savings in Medicaid.
Talcove said the federal government could obtain $1 trillion in savings through three steps:
- Validating applicants identity on the front end
- Eliminating self-certification
- Monitoring the backend of benefit programs through improved technology
Without such steps, the ability of foreign criminal organizations to use technology to falsely enroll and bill Medicaid will continue to proliferate, he said.
“The people that are stealing information now, I believe, are ghosts,” Talcove said. “They are ghosts from China, Romania.”
The imperative for an aggressive federal push to cut fraud was not only the federal government’s $37 trillion debt, which it is increasing by $2 trillion annually. Additionally, Republicans highlighted projections by the Economic Policy Innovation Center that the federal government is headed for its fiscal limit, or the maximum debt-to-GDP ratio beyond which the government cannot stabilize its finances using its historical pattern of fiscal adjustments.
“We’re at the precipice of a debt cycle and dollar [being] devalued and worth nothing,” said Rep. Eric Burlison (R-Mo.).





