Direct-to-employer benefit design: A providers’ starter guide
A leading health system in the Southeast has found that partnering directly with employers on value-based benefits is an effective strategic response to soaring healthcare costs.
Following a decade of experience in developing value-based care bundle programs, Nashville, Tenn.-based Vanderbilt University Medical Center (VUMC) has enjoyed success in direct contracting with employers that demonstrates the ripe market opportunity such contracting offers. Health systems that want to seize this opportunity can benefit from applying VUMC’s lessons learned during this process to their own circumstances.
The significance of the opportunity is clear based on current trends. Employers face a projected 9% to 10% increase in healthcare costs during the 2024-26 contract renewal period.a This increase is compounded by the surge in healthcare utilization post-COVID-19 and the growing prevalence of expensive chronic conditions.
Many employers, enticed by the promise of value-based care for better outcomes at lower costs, have been looking to integrate these solutions into their benefits programs.b For some, this strategy means partnering with their local health system.
Health systems that can successfully create and launch direct-to-employer health benefits can produce a win-win for all parties involved, including not only employers, employee-patients and providers but also the nation’s healthcare system as a whole.
To successfully build its direct-to-employer contracting programs and, ultimately, launch its benefit product commercially, VUMC began with a focus on three crucial steps: redesigning care delivery, aligning payment models and developing the means to track and monitor performance.
1 Redesigning healthcare delivery
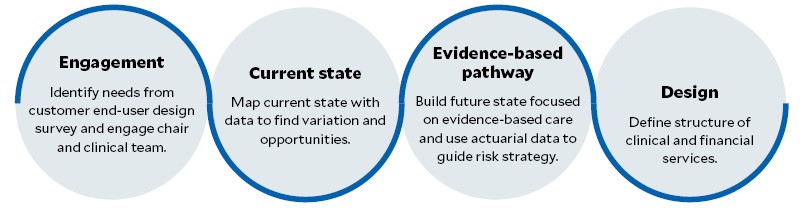
Establishing a new form of healthcare business requires time to gather expertise and test. It is not simply a matter of treating the finances differently. Structural change must take place, and to effectively accomplish that change, health systems must first understand their market opportunities, the needs of patients and employer’s pain points. They then must connect with their clinical teams and fully adopt an evidence-based approach to healthcare. Details regarding each of these steps are as follows.
Map the target market to find variations and opportunities. A health system may find its market lacks sufficient maternity care options or discover that many employers are seeking value-based care for employees’ orthopedic needs. Health system leaders should consult with an actuarial expert who can help them understand how much utilization is in the market and guide the organization’s level of risk.
Understand patient needs. Organizations can best gather data from patients using a simple end-user survey.
Identify employers’ common pain points. Hospitals and health systems are employers, too, which helps them understand and relate to the unique challenges that other employers face. As Tennessee’s largest private employer, VUMC leverages its experience managing the diverse needs of its own employee population to benefit the region’s employers and bring insight and solutions to industries of all sizes and shapes.
Connect with clinical teams. A VUMC priority was to engage clinical teams in benefit-design sessions to help them understand and map out the optimal patient journey and experience.
Engaging clinical teams is critical to keeping patients at the center of care. If the focus is on delivering the best outcomes, costs will come down. As part of this engagement, clinicians should be asked to identify actions they would want to take during care and to be specific as they scrutinize every aspect of the patient journey — from clinical aspects such as post-procedure care to patient experience details such as parking instructions. Health system leaders should conduct focus groups or one-on-one sessions with clinicians to motivate them to speak freely about how processes can be efficiently redesigned to produce the best possible clinical outcomes.
Implement an evidence-based design. The health system should seek to build a future state focused on evidence-based care, with the payment model wrapped around the clinical pathway using actuarial data to guide how much risk to tolerate. Stakeholder feedback and market data should be synthesized to provide the basis for creating evidence-based programs. Patient thresholds and quality measures should be established in consultation with clinical teams.
Elements that should be addresses in developing an evidence-base healthcare design
2 Aligning payment with clinical redesign
After redesigning care delivery to drive better health outcomes, the next phase is to tie payment to redesigned clinical workflows by adopting a payment model that embodies financial incentives to match risk. Under this model, payment should be designed to reward delivery of the right care, not just more care. For example, in its bundle for maternity care, called MyMaternityHealth, VUMC takes on risk by setting a target cesarean-section rate and taking a payment reduction if it misses the target.
3 Measuring and tracking performance
Health system leaders should regularly monitor progress on patient thresholds and quality measures, with the clearly stated expectation that regular adjustments may be necessary.
It is important to maintain ongoing communication with clinicians after a benefit is created not only because it will be necessary to monitor their level of engagement but also because the process will require continuous improvement and adaptation as the industry evolves.
VUMC has set up channels and platforms for employers and patients to regularly submit their feedback on their experience, and feedback is communicated to providers in as close to real time as possible. Creating a consistent feedback mechanism helps to reinforce positive processes and to correct unhelpful approaches.
4 A key ingredient: Reward high-value care
Through its direct contracting efforts, VUMC has found that patients achieve the best health outcomes when providers have the resources and incentives to deliver optimal care. Value-based care empowers providers to operate at the top of their license and offer proactive health services.
VUMC also has found that early interventions and more strategic, focused care at the start of a patient’s journey reduce the likelihood of costly claims later. For example, in its MyMaternityHealth bundle, identifying complications early has allowed for timely interventions, avoiding the inefficiencies and tedious insurer negotiations.
Value-based care also enhances population health management. In VUMC’s case, efficient, streamlined workflows have not only ensured patients receive the best care but also led to significant cost savings for everyone involved.
5 Implementation strategies
Based on VUMC’s experience, health systems preparing to launch their health benefit program commercially would benefit from a focus on the following strategies.
Strengthen the organization’s financial infrastructure. Health systems should take steps to ensure their financial systems are robust enough to handle the fluctuations of a rapidly evolving industry and the changing demands of patients.
Cultivate employer partnerships early. Health systems should work to build strong relationships with employers from the outset by actively involving them in the program design process. Their input can help the organization tailor its offerings to better meet their needs and foster long-term collaboration and trust.
Create a comprehensive marketing strategy. A detailed marketing plan is needed to effectively launch an employer-focused health benefit program. To ensure a successful rollout and ongoing engagement, the plan should identify the target audience and include a market analysis, branding, communication strategies and performance metrics.
Learn from successful implementations. Health system leaders should seek advice and insights from organizations that have successfully transitioned to their own health benefit programs. Their experiences can provide valuable lessons, helping the organization to avoid common pitfalls and replicate best practices.
Continually assess and improve the program. Health systems should evaluate their programs on a regular basis to make sure the clinical pathways are up to date and the patient experience is exemplary. VUMC has been inspired by feedback from patients, employers and providers to make changes to its MyMaternityHealth program, for example, such as adding new locations and new service codes to the definition of the bundle.
Both listening and responding to feedback are critical for ensuring a program will grow and evolve to meet the needs of patients and the market.
Footnotes
a. Gupta, A., et al., “Reimagining US employer health benefits with innovative plan designs,” McKinsey & Co, Oct. 15, 2024.
b. Roesler, A.R., Totten, A., and Kocsis, S.W., Reimagining the future of employer-sponsored health care to drive value: Survey insights, Milken Institute, May 5, 2024.





