Where do we go now? Action needed to address public dissatisfaction with U.S. healthcare
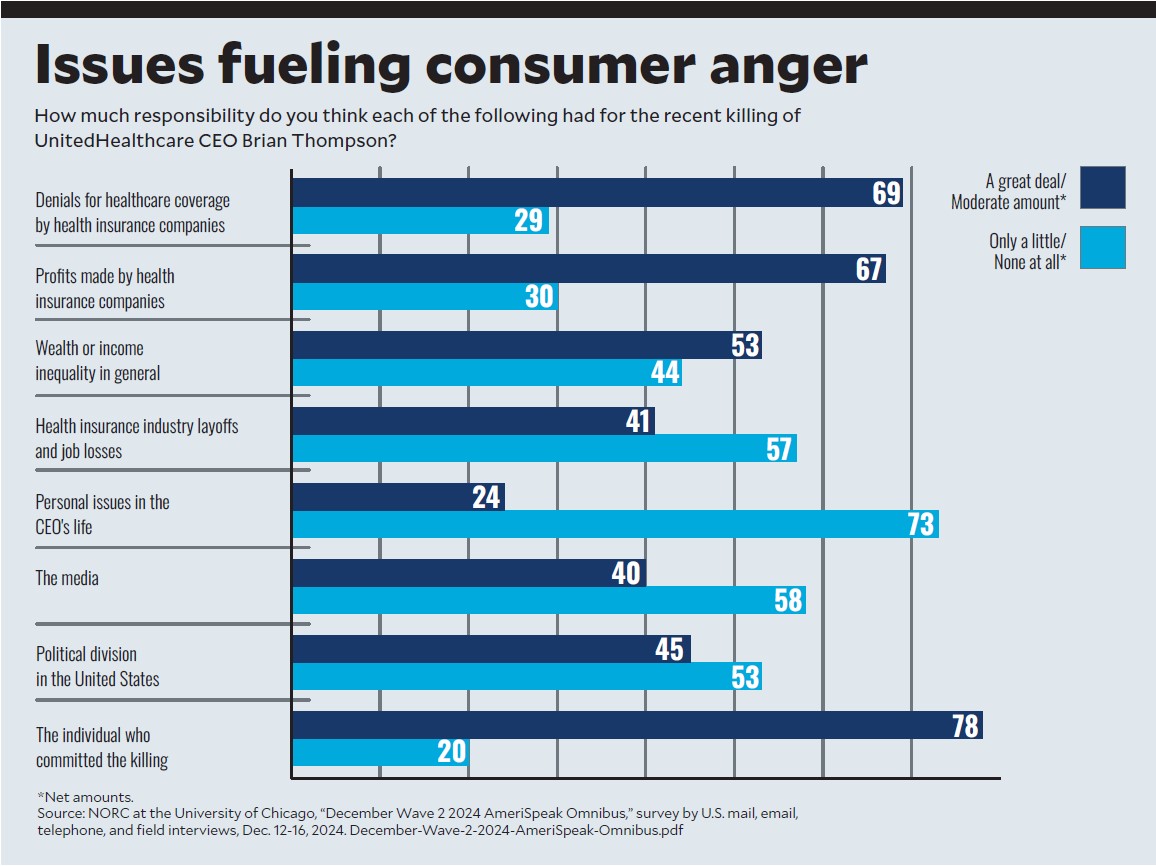
The public response to the murder of UnitedHealthcare’s CEO underscores the widespread public dissatisfaction with the healthcare system. Industry leaders say it’s time for action.
Amid a wave of public anger directed at the healthcare system, provider organizations are examining their approaches to understanding and responding to mounting discontent.
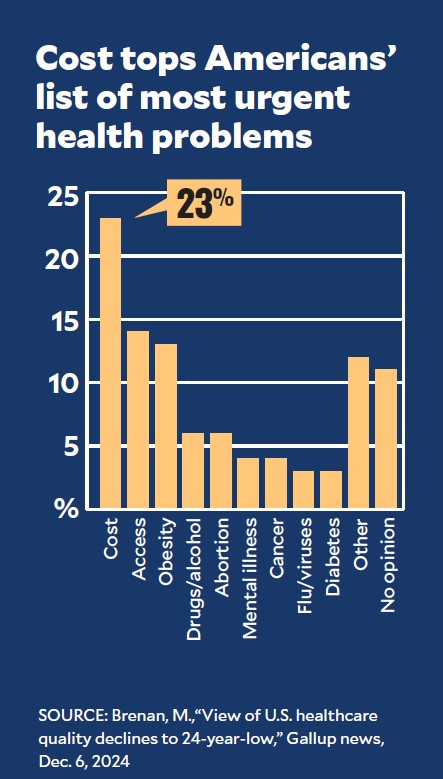
Even as insurers have incurred the brunt of criticism in public forums, including in the aftermath of the Dec. 4 murder of UnitedHealthcare CEO Brian Thompson on a Midtown Manhattan street, the most pervasive concerns extend more broadly.
“Many of us in the healthcare field have seen the tension growing,” said Rick Gundling, FHFMA, CMA, senior vice president for content and professional practice with HFMA. “We talk about the payer-provider divide, but unfortunately, it’s the patient who falls into that divide, too.”

It’s all of our responsibility,” said Cheryl Matejka, MBA, executive vice president and CFO for
Mercy, a 50-hospital health system.
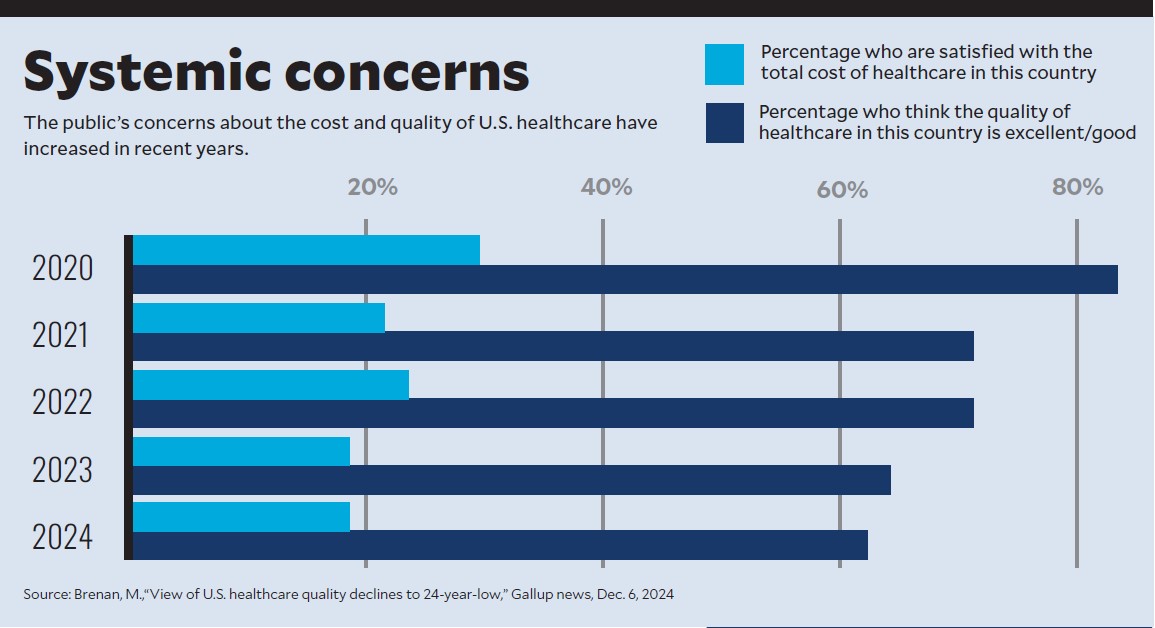
Although some of the online commentary after Thompson’s death crossed a line into indecency or crassness, Gundling said the underlying emotion should be heeded. It signals an increasing lack of confidence in the system, as is also suggested by results of a November poll conducted by Gallup.a
More than half (54%) of the 1,001 poll respondents rated healthcare quality as fair or poor, the worst mark in 24 years, while 70% said the system has major problems or is in a state of crisis. Muddying the picture, however, 71% rated their own healthcare as excellent or good, as did 65% for their own health insurance.
Even if some data points suggest optimism about the industry, healthcare leaders say it would be a mistake to overlook the broader trends.
“We’re driven to get healthcare right. Address access, affordability, eliminate friction. It’s all of our responsibility,” said Cheryl Matejka, MBA, executive vice president and CFO for Mercy, a 50-hospital multistate system headquartered in Chesterfield, Mo.
Matejka and other industry leaders say there are a number of ways for organizations to address key areas of concern.
Improve access
Mercy uses various engagement tools to aggregate feedback from patients and clinical staff. Access-related issues are a central theme that has emerged from those listening posts, Matejka said.
“What we hear from our patients is they want access now, and on their terms,” Matejka said.
The organization has initiated several strategies to promote optimal access, including by more comprehensively deploying advanced practice providers and virtual care.
In addition to mandatory instruments such as HCAHPS, Mercy utilizes third-party research on consumers’ feelings about their healthcare, plus specialized research on
consumer-centric behavior. The insights helped nudge Mercy to deploy enhanced self-scheduling technology. (See the sidebar below, “Identifying pain points that rankle consumers is critical” below for more on capturing consumer sentiment.)
“That’s a way for patients to feel empowered,” Matejka said. “They can control the ‘where’ and the ‘when,’ and do many things that they do on their phone in other industries.”
AI will be the farthest-reaching solution to access-related issues, a particular patient pain point, especially as the population ages, said Dennis Dahlen, FHFMA, MBA, CPA, the CFO of Mayo Clinic and past HFMA National Chair. Mayo is partnering with a leading chipmaker to revolutionize how medical pathology is practiced by employing digital imaging and AI.
View inability to pay as a never event
A shortcoming in revenue cycle processes that can reflect poorly on hospitals is the prevalence of patients who are eligible for charity care yet don’t receive it, said Eli Rushbanks, JD, general counsel and director for policy advocacy at the consumer advocacy group Dollar For.
In his organization’s survey results from late 2023, 29% of patients with hospital bills they could not afford were able to learn about, apply for and receive charity care.b The biggest obstacle was lack of awareness among respondents that charity care was an option, Rushbanks said.
Hospitals should consider a failure of an eligible patient to receive charity care as a “never event,” he said, similar to how certain breakdowns in clinical processes are viewed.
“If they treated a patient getting sued for money who was eligible for charity care [like a never event], a lot of this would get fixed,” Rushbanks said.
“Instead of just saying, ‘We did what we were supposed to do. The patient didn’t meet us in the middle,’ [we should be] saying, ‘Why aren’t patients filling out the charity care application? Maybe we need to ditch the idea of an application. Maybe we need a presumptive eligibility model.’”
In such a model, he noted, hospitals would benefit from easy access to government databases that allow for income verification.
Health system leaders are wary of taking on unilateral responsibility for making prices more affordable at a time when their costs are high and reimbursement from government payers fails to cover those costs. Steps being incorporated by providers such as Mercy and Mayo Clinic include working to address the total cost of care by sharply focusing on population health and offering maximum flexibility in payment plans.
In late 2023, Mayo Clinic halted legal action in most collection scenarios. Dahlen said a comprehensive review of processes showed that the net collections from such action “wasn’t significant, so we discontinued using these methods except in extreme circumstances,” such as when a patient has received insurance benefits to cover the care yet will not pay.
Resolve administrative snags
Many issues that hinder access are beyond the scope of providers to fix by themselves.
“A lot of our work with payers has focused on the need to eliminate friction in the care process,” Matejka said. “And that [friction] typically happens either when the care is being scheduled or it’s being transitioned to the next level.”
Mercy pushes for programs such as gold carding, which involves taking steps to highlight providers that have a history of furnishing high-quality, cost-effective healthcare and enabling them to practice with fewer payer restrictions. The organization also plans to build on its track record of engaging in direct contracting with employers.
At Mayo Clinic, negative patient feedback tends to be based on holdups in care delivery stemming from prior authorization, Dahlen said.
Even as patients are set to travel to the campus for their service, the insurer has not granted approval. Complaints also arise from clinical denials and network-based denials, he said.
A master playbook or inventory of clinical conditions that justify particular procedures or treatment regimens would go a long way toward streamlining authorization, if providers and insurers can agree on how to compile such a resource, Dahlen said.
“If we have to argue about it, let’s argue about it upfront, not with a patient in the middle,” he said.
Navigate coverage issues
Roadblocks to receiving healthcare are not the only source of consternation about health insurance. Confusion abounds regarding the fine print of health plans.

insurance coverage and what your risks are is high,”
said Paul Keckley, PhD, a healthcare policy analyst.
“The level of mass ignorance about what’s in your insurance coverage and what your risks are is high,” said Paul Keckley, PhD, a healthcare policy analyst and managing editor of The Keckley Report.
Just because all relevant benefits information is available online doesn’t mean it’s genuinely accessible.
“Knowing how to navigate in with only two clicks to get the information you need is the secret sauce,” Keckley said. “And that’s not done yet.”
An optimal tool would allow prospective enrollees to gauge their likely out-of-pocket costs — based on their health status, conditions and medications — versus the monthly premium for the plan, said Heather Stallings Dunn, CHFP, CRCR, MBA, president of SSI Group.
That would help with plan selection, but education would need to continue because of the complexity of the terms and conditions. For example, Dunn noted that a commonly asked question is why there was a charge for a colonoscopy, supposedly a free preventive service. The problem is that if an issue is found, the procedure becomes categorized as diagnostic rather than preventive.
Identifying pain points that rankle consumers is critical
The first step in addressing consumer discontent with the U.S. healthcare system is to precisely understand the root causes. Leading healthcare providers have adopted various tools and tactics to parse consumer feedback in ways that can spur constructive changes.
Missouri-based Mercy draws on third-party research from organizations such as Gartner and Advisory Board that speaks to overall feelings about the industry, said Cheryl Matejka, MBA, executive vice president and CFO. The health system also makes a point of utilizing insights from studies of consumer-centric behavioral research conducted by organizations such as Kaufman Hall.
“Understanding the challenges that consumers are facing, what’s preventing them from seeking healthcare or connecting to the care they need, is critical to help us design and build a next-generation care model that makes it easy for those we serve to both engage and feel empowered to do so,” Matejka said.
At Corewell Health in Michigan, all team members have access to a platform where they can enter information about any type of consumer-facing or process-related issue or problem, said Sarah Clark, vice president for registration and financial counseling. Relevant reports on the subject are circulated daily to team leadership and in aggregate summaries for system leadership.
“Even though we’ve tried to educate patients about situations like that up front through estimates and language on pre-procedure documentation, it’s not working and leaves patients and providers who have to collect from the patient frustrated,” Dunn said.
Push for transparency
Price transparency is prominent among the areas of healthcare where regulations do not yet translate to worthwhile policy and outcomes.
“We’re disclosing, we’re doing transparency, but not in a way that makes it easy for [everyday Americans] to understand it,” Keckley said.
Some providers are striving to get ahead of the curve, recognizing that although patients may not be delighted by their bill in any case, if they understand it ahead of time, they’ll be a lot more likely to accept it.
Corewell Health, a 22-hospital, Michigan-based system, has updated the verbiage in its estimate letters and point-of-service scripting “to aim at leading with trying to educate [patients],” said Sarah Clark, CRCR, vice president for registration and financial counseling.
At Main Line Health outside Philadelphia, good-faith estimates include co-providers when those providers are employed by or formally aligned with the health system, said Johanna Weller, MBA, system vice president for revenue cycle. A vendor helps the estimates pinpoint the patient’s projected out-of-pocket cost.
But providers that have no formal contractual relationship with the health system are excluded.
“I cannot give the patient a good faith estimate for anesthesia,” Weller said as an example. “Having to explain all of that to patients has been a challenge.”
The estimates not only represent a greater focus on transparency in the years since federal regulations went into effect in 2021, but also are part of an evolution in financial counseling. Weller’s team has shifted human resources to interact with patients on the front end of the revenue cycle, taking a more electronic approach to the back-end processes.
Examine public relations
The online vitriol that followed Thompson’s killing also reflects heightened antagonism toward executives in general, Keckley said.
Organizations thus should be thoughtful about how their executive compensation is portrayed to the public at a time when policymakers can be expected to push to make that information more widely available. Governance boards, which set executive compensation, should consider how to communicate the criteria to communities.
“The reaction has been [to] kind of hunker down: ‘This was a senseless and unfortunate problem,’ which many would say is more a United or health insurance problem than it is for the rest of us,” Keckley said. “I happen to disagree with that. Any celebrity CEO, and especially those that are investing a lot of money making sure their name, brand and image [are] out there, they’re vulnerable.”
Public relations teams increasingly may be called on to monitor and respond to specific allegations about an organization or executive in social media forums,
Keckley added.
Given that such efforts can’t stem every potential threat, organizations also can consider evaluating their security procedures. For example, Corewell Health employs a position that’s trained to dually serve in a security and a registration intake role in the system’s ambulatory buildings.
Since the position was added, Clark said, workers feel safer, and the number of safety events has fallen in those facilities.
Don’t wait to act
The angst being expressed about the U.S. healthcare system makes for easy political fodder, raising the likelihood that Congress or federal and state regulatory agencies will seek to implement policy mandates. One way to limit any such outcome is for stakeholders to take the lead.
“The message of [the] public outpouring is something we can [use to] take action for all parties — providers and health plans — to establish a better baseline for a collaboration and partnership,” Gundling said. “This will build overall public trust.”
Footnotes
a. Brenan, M., “View of U.S. healthcare quality declines to 24-year low,” Gallup, Dec. 6, 2024.
b. “The path to charity care: exploring the journey and roadblocks to financial assistance for medical bills,” Dollar For, accessed Jan. 10, 2025.
Prior authorization draws scant concern from the public
Healthcare providers have raised alarm that the expanding use of prior authorization (PA) creates outsized harm on patient care, but recent polling shows there’s much less interest from patients.
A survey published in September in Health Affairs Scholar found:a
- 34% of patients saw no PA burden
- 7% of payers saw no burden
- 2% of providers saw no burden
Seventy-six percent of patients perceived the PA process as being efficient.
“Patients are generally not dealing with PA often, let alone daily like many providers and private payers. Effectively, patients shift much of the effort to providers and private payers,” wrote researchers from Harvard, McKinsey & Co., Stanford and the National Bureau of Economic Research.
Paul Keckley, PhD, healthcare policy analyst, said he was not surprised, saying, “That’s more hospitals and docs taking shots at the plans. Surprisingly, no one is taking shots at the plans for premiums or in- and out-of-network provisions that could be a big difference in how much you end up having to pay.”
Footnote
a. “Perceptions of prior authorization burden and solutions,” Health Affairs Scholar, September 2024.





