The Healthcare C-Suite of the Future: From AI to ROI–Emerging needs drive demand for new skillsets
Survey finds health system leaders feeling underprepared.
With support from:

In an era of unsustainable costs, rapid technological advancement and the push for greater ROI from the healthcare dollar, the old ways of doing business in healthcare are doomed to failure, industry experts say. This puts C-suite leaders in the hot seat, testing their ability to make the right decisions for their organization’s future.
“There have to be new mechanisms — mostly technological — that allow you to deliver better, safer and more accessible care at a lower cost,” said Robert Wachter, MD, professor and chair of the Department of Medicine at the University of California, San Francisco, and author of A Giant Leap: How AI is Transforming Healthcare and What That Means for Our Future.
New tools like AI are poised to radically transform how decisions around diagnosis and treatment are made. But the level of change taking place also raises the stakes for leaders in determining where to invest, how much money to direct toward AI innovation and how quickly to adopt AI use cases. Moving too fast too soon puts organizations at risk — yet there’s also a risk that comes with inaction.
The question then is: Are healthcare C-suite leaders equipped to guide their organizations to survive and thrive in the coming transformation?
“People in the C-suite didn’t learn this in C-suite school,” Wachter said. “They need to understand the technology and how it works, how to evaluate it and how to separate the hype from the reality. They also need to build a governance structure and surround themselves with the right people to weigh their options.
“The technology is not that hard to leverage,” Wachter said. “Getting it right frequently enough that you build trust in the tools is quite hard.”
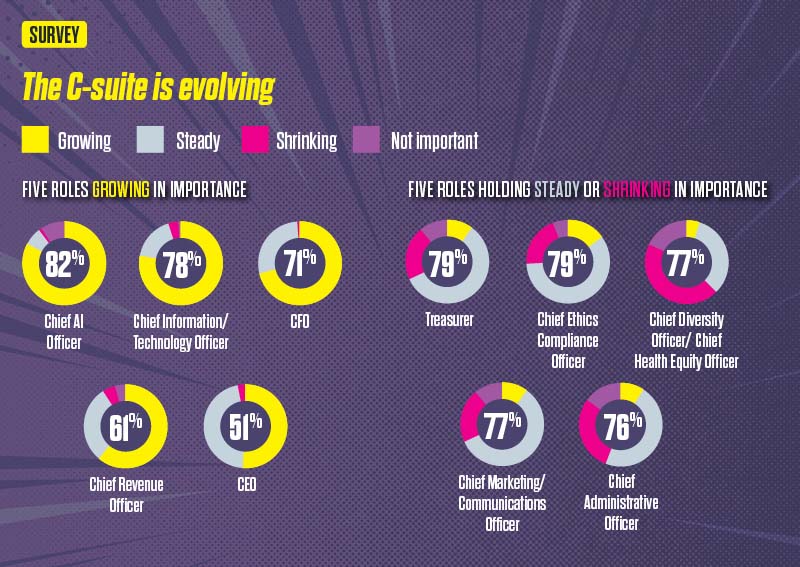
The range of responsibilities that healthcare C-suite leaders now shoulder is growing, which reflects the pace of change in the industry.

“When I think about the healthcare C-suite of the future and the skills and capabilities that are going to be important, understanding data and developing fluency around AI and how it’s going to change our work will be key,” said Robin Damschroder, president, value-based enterprise, and CFO for Henry Ford Health, based in Detroit.
“It can’t just be a few people in the organization who understand AI. We’re all going to have to understand how it works, down to the director level, because this is going to be driving a lot of the workflow,” said Damschroder, an HFMA board member.
An HFMA survey of healthcare CFOs and other C-suite leaders found strategy and leadership skills are rising in importance, followed by skills in technology and organizational communications. Meanwhile, new, must-have capabilities are emerging — especially in the areas of innovation and transportation, AI competency, digital technology and payer relations.
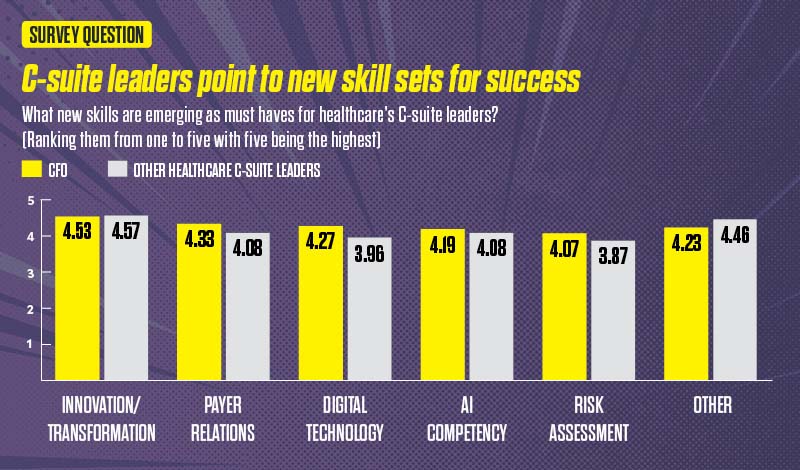
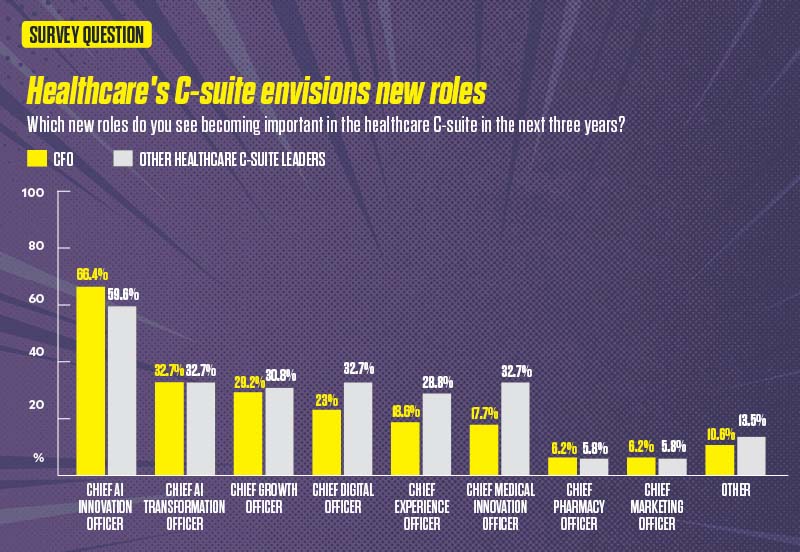
Note: Chart data obtained from an HFMA survey of healthcare leaders, with 125 CFO and other 57 C-suite leaders participating. Respondents could select more than one response.
Can today’s hospital and health system leaders respond?
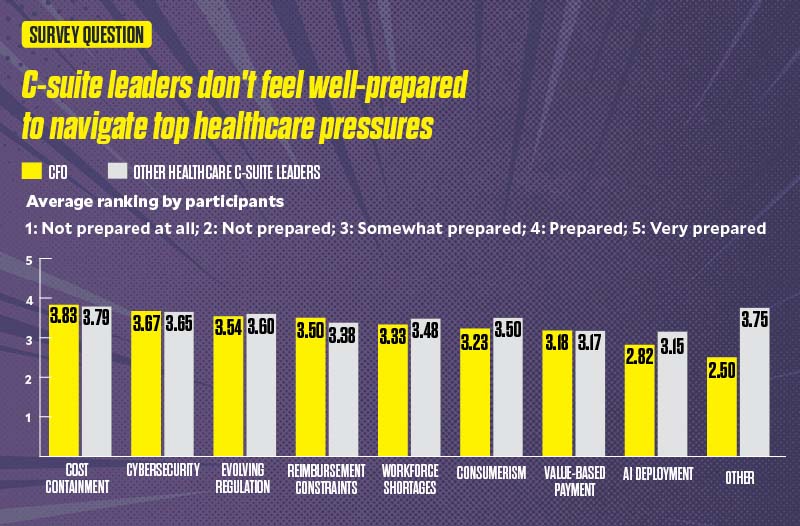
As leaders face a growing list of pressures, there are signs that the responsibility they feel to respond in the right ways at the right time weighs on them. Across titles, senior healthcare leaders don’t feel strongly prepared to navigate the industry’s top challenges, from a rapidly changing regulatory environment to cost and reimbursement pressures to demands from consumers and other purchasers.

And when it comes to AI deployment, CFOs feel even less prepared to lead this transformation than other C-suite leaders, ranking their confidence level at 2.82 on a scale of 1 to 5. (See exhibit, below.)
“This is what it feels like when the model starts breaking down,” said Dan Liljenquist, senior vice president and chief strategy officer, Intermountain Health, based in Salt Lake City. “With a multi-trillion-dollar national debt and the acceleration of annual deficits, the United States simply cannot afford the healthcare system we have today. The financial pressures are mounting, and reality is not negotiable.”
Liljenquist said navigating these pressures will require “creativity and a lot of curiosity” to shape a future-forward outlook on what’s next and what’s needed in healthcare.
“We need leaders who are willing to challenge their own assumptions and lean into learning,” he said. “The external headwinds — whether from macroeconomic disruption, regulatory shifts or technological transformation — aren’t coming. They’re already here. And the organizations that will thrive are those that can adapt in real time.”
Pressure increases on healthcare C-suite leaders
The ability to articulate what the future of healthcare could or should look like and prepare their teams for what’s coming has never been more crucial among healthcare C-suite leaders.
“We have to be more aggressive at setting a vision and then the agenda to get there,” said Alex Maiersperger, global product marketing lead, healthcare, SAS, and host of the company’s podcast, The Health Pulse.
“I think the biggest challenge right now is you have some leaders [who say], ‘This is how it is. This is what you’re doing. Here it is.’ And for so many on their teams, it just feels like they’re not a part of progress.”
Among healthcare CFOs in particular, there is increased focus on strengthening enterprise value — and it’s a team sport, according to Henry Ford’s Damschroder.
“For CFOs, I think the focus has shifted from ‘What can I do in my areas to help advance and support operations?’ to really looking around and asking, ‘How do I collaborate with my peers to create enterprise value?’ with a focus beyond financial stewardship and capital budgets,” Damschroder said.
That shift is changing how C-suites function.
“They’re digging into the clinical outcomes, consumer experience, the total cost of care — things that we all measure together and are incented on — and really figuring out ways to support that work,” Damschroder said.
At the same table during discussions on risk-based arrangements or value-based care models, there are team members who specialize in population health, payer strategies, operations and process design, she said. Intentional effort goes toward redesigning workflows to complement new technologies, with a focus not just on efficiency, but also on reimagining tasks to bring joy back to work.
Key areas for innovation
In conversations with healthcare C-suite leaders and through open-ended survey responses, leaders explored priority areas for innovation in a transformative environment. Three areas rose to the top of leaders’ lists.
1. AI and automation. Today, 85% of healthcare providers, payers and technology groups are exploring use of the AI tool ChatGPT or have already implemented it in some way, according to a McKinsey & Co. survey.a The ROI for incorporating AI and automated tools is projected to be significant. A PwC study estimates the healthcare industry could reduce healthcare spending by $1 trillion over the next decade by reducing fragmentation and emphasizing a digital-first, proactive, personalized system of care, including through the use of AI and automated tools.b
“Healthcare is always constrained by workforce supply, and automating processes, enhancing clinical decision-making and enhancing operating efficiencies can all relieve the stress on the demand for labor,” one CFO survey respondent said.
A call to action for C-suite leaders is to concentrate on strengthening AI fluency for themselves and their teams.
Wachter believes AI’s largest influence on healthcare will occur when AI begins to intervene in and even make decisions around diagnosis and treatment. Meanwhile, C-suite leaders point to its strong potential to reduce administrative expense and drive efficiency gains. They also highlight the need to integrate AI with patient-facing offerings.
2. Ambulatory care. Also a top focus for CFOs as they look to the future: developing the right strategy around ambulatory care. Today, home-based care and outpatient services, including in ambulatory centers, are projected to be the fastest-growing care sites through 2034, according to Kaufman Hall, a Vizient Co.c
Amid this shift, building the right mix of services and ensuring these services are staffed appropriately despite ongoing workforce challenges will prove critical.

“Given the way ambulatory is growing, how do we make sure we have a dedicated focus that not only supports the hospital, but also supports our health plan?” said Melinda Hancock, executive vice president and CFO for Sentara, a large nonprofit integrated health system based in Virginia.
3. Payer-provider relations. For C-suite leaders as a whole, expertise in payer relations, too, is viewed as key to an organization’s financial sustainability. In 2024, an HFMA survey found nearly 58% of healthcare finance leaders believed their organization’s relationship with payers had become “somewhat negative” or “mostly negative” during the previous three years. Finance leaders speaking at HFMA’s Thought Leadership Retreat in September said they hadn’t seen improvement in payer-provider relations. If anything, relations have “gotten worse” in the past year, some said.
For that reason, proactive C-suite leaders are taking a close look at what is needed to drive better outcomes at lower cost and how to partner with payers. They also are considering what resources are needed to support population health and how to hone risk-management capabilities related to value-based care.
“If you’re going to drive down real costs on the clinical delivery side, you have to understand the contract mechanics, how risk gets attributed to you, and really what’s [driving] the prioritization of clinical care redesign,” Damschroder said. “That’s what we’re spending a lot of time doing.”
As the list of features considered crucial to health systems’ success grows, there has been an explosion in C-suite titles, such as chief AI implementation officer, chief experience officer and chief of ambulatory virtual care officer.
“We’re really seeing that evolution continue to happen,” said Jena Abernathy, senior client partner, CEO & executive search, and sector lead, healthcare board services, Korn Ferry.
Today, just 47% of healthcare CFOs believe we’ll see fewer leaders in healthcare C-suites in the future, the HFMA survey found.
Typically, as healthcare C-suites and boards look at the composition of senior leadership teams that will be needed to lead their organizations into the future, they focus on a three-year window. That’s because of the pace of new regulations being introduced, the rate at which new cost pressures are emerging and the acceleration of advanced technologies entering the market. The chief observability officer — a new role Abernathy is seeing in healthcare — emerged from the need to evaluate the ROI of digital technology investments.
One C-suite title healthcare organizations aren’t seeing as much of is that of chief diversity officer. The responsibilities that fell under this role typically have been absorbed by other positions or fall under roles that are new to healthcare: the chief health equity officer or the chief community officer, according to Donna Padilla, executive partner and market leader, healthcare, for WittKieffer.
Team building takes center stage
Among the healthcare CEOs the Oak Brook, Illinois-based executive search firm WittKieffer has spoken with, there’s an emphasis on bringing on leaders who demonstrate a learning mindset. It’s considered critical to a team’s ability to adapt in a fast-paced environment.
“CEOs really articulated, ‘How do we go from being frenetic to also being visionary?’ And quite frankly, that’s how teams have to think, too,” Padilla said.
Increasingly, Padilla is also seeing CEOs and boards assess candidates for adaptability and emotional intelligence, as well as an understanding of how their actions impact their team.
“There’s more mindfulness around the idea that if you’ve got a team that looks like everything’s on fire all the time, you start to exhaust the team around you and the team around them,” Padilla said.
There is a danger to building a C-suite that becomes so large it becomes difficult for a CEO to manage team dynamics and have a pulse on the team’s efforts, individually and collectively.
“When you think about span of control for a CEO, you want to be really careful about how many roles you add and make sure that it’s accretive and that you’re driving accountability,” Abernathy said. “You want to be sure that everyone is aligned with where you’re headed and what you’re trying to accomplish from a strategy and business perspective.”
At Sentara, Hancock formerly served as chief transformation officer. She codeveloped the health system’s strategy for investment, uncovering opportunities for clinical and operational innovation without pulling from the organization’s operating margin.
One key lesson learned, according to Hancock: “Understanding that you can’t do innovation off the side of your desk. It needs a dedicated role.
“We [as leaders] love focusing on innovation. None of us wanted to give it up,” she said. “And it is fun to meet with companies to see the technologies they’ve developed to improve how we interact with patients or the patient record. It’s really fun, cool work. But as a leader, you have to understand when to say, ‘OK, as much as I love this, I’m not giving it the full attention it deserves for the future of my company.’”
Power duo relationships emerge
As C-suite leaders take on their organization’s toughest challenges, the industry is seeing more intense collaboration among C-suite roles.

“We’ve actually quantified the operating efficiencies we have to find,” said Patricia Steeves O’Neil, MAE, senior vice president and CFO, Rush University System for Health in Chicago. “We’ve quantified the growth we need to find. So the good news is we have that information. Now, it’s all in the implementation.”
As O’Neil looks for ways to tackle labor supply challenges — an area where costs are growing at a higher rate than revenue — she partners closely with Rush’s chief human resources officer (CHRO) around labor strategy.
“When 50% of all of your operating expenses go toward labor, there has to be alignment not just on controlling the expense, but also, ‘What’s our nurse staffing model? Do we insource? Do we outsource? What benefits do we provide?’” she said. “And so I’ve seen a much tighter alignment between me and the CHRO and our teams.”

C-suite leaders responding to HFMA’s survey highlighted the leaders with whom they partner most closely. For CFOs, these “power duo” relationships are most likely to exist between the CFO and the treasurer, chief marketing officer or chief investment officer.
For Dominique Wells, RN, MSN, COO of Conduit Health Partners, a nurse-led subsidiary of Cincinnati-based Bon Secours Mercy Health, her relationship with the organization’s CFO ranks among the most important.
“I’m closely aligned with our CFO — we work hand in hand,” said Wells, who began her career as a hospital housekeeper before advancing to leadership. “And every decision that I’m thinking about or exploring, I’m constantly bringing the CFO in to drive optimization and efficiency, she said. “Being able to use financial insights as some of the basis for that decision-making helps us align our focus.”

Given the weight of consumer expectations in healthcare as well as the need to more actively involve consumers in managing their health, strong partnerships between CFOs and chief marketing officers have become vital, according to Geeta Nayyar, MD, MBA, chief medical officer for San Francisco-based RadiantGraph and an HFMA board member.
“We’ve really never thought of marketing as critically important to the business of health-care,” Nayyar said. “But in the growing era of misinformation and disinformation — in the growing era of ‘Dr. TikTok’ now being the new competitor to hospitals — marketing is actually patient engagement. It’s patient acquisition, retention, brand loyalty, trust.”
Damschroder, meanwhile, spends a lot of time with her organization’s chief physician executive, especially in her role as president of Henry Ford Health’s value-based enterprise and the physician executive’s dual role as president of the health system’s clinical delivery system.
“That’s a significant duo,” Damschroder said.
Hancock believes strong relationships with all C-suite leaders are vital. She finds herself increasingly working with the system’s chief consumer officer so the system makes financial decisions in the best interest of consumers.
Maintaining a future focus
With so much of healthcare in flux, how can existing and new C-suite leaders prepare to lead their organizations? The best leaders are good at connecting the dots, O’Neil said.
“I think the ones that really succeed have an understanding of the macroeconomic environment and are not living in sort of this internal bubble. They understand the risks; understand the need for prioritization,” O’Neil said. “We can’t say yes to everything, which is sometimes hard.”
The key is knowing when the risk of not doing something is greater than the risk of making a move or investment, she said. Those are decisions that are more easily made with data, collaboration and experience.
Wells, meanwhile, urges new C-suite leaders to let go of their fear of the unknown.
“I always go back to not being afraid,” she said. “I tell people, ‘Be bold. Raise your hand, even when you think that you’re not ready. The more exposure you have, the better you’ll be able to prepare and jump in at those pivot points.’ And we see the C-suite pivoting constantly.”
Footnotes
a. Martin, C.P., et al., “Generative AI in healthcare: Current trends and future outlook,” McKinsey & Co., March 26, 2025.
b. “From breaking point to breakthrough: the $1 trillion opportunity to reinvent healthcare,” PwC, Sept. 17, 2025.
c. Hulstrand, R., “Redesigning ambulatory care for what’s next,” Vizient, Aug. 5, 2025; and “Outpatient shift turning to new specialties,” Gist Graphic of the Week, Kaufman Hall, July 12, 2024.





