CMS implements policies to cut $50 billion in federal healthcare spending
Administrator Mehmet Oz was seen as prioritizing aggregate CMS cost reduction.
CMS, under its new administrator, has implemented policies estimated to cut more than $50 billion in federal spending on Medicaid and Medicare, according to a recent analysis.
The savings derive from new policy directions overseen by Mehmet Oz, MD, administrator of CMS, said Chris Pope, a senior fellow at the Manhattan Institute, a right-leaning think tank who has advised leaders appointed to lead the current CMS.
Reductions in federal healthcare spending, according to his calculations, include:
- Possibly $11 billion in 2026 through a proposal to tightening oversight of enrollment in the ACA plans
- Up to $25 billion from closing a loophole states used to garner federal matching funds for Medicaid
- $3 billion for Medicaid by barring (pdf) payments for social determinants of health
- $4 billion (annualized) from withholding (pdf) Medicare coverage for weight-loss drugs, at least for now
- Less than $1 billion from increased targeting of overpayments to Medicare Advantage plans
Another $10 billion in annual Medicare spending on skin substitutes was targeted through rule changes, although Medicare rules require those savings to be offset by other Medicare spending.
“What we’re seeing is Oz is actually a fiscal conservative,” Pope said in an interview. “And he’s been pretty effective in pursuing that.”
Oz, confirmed in April, has instituted policy changes much more rapidly than CMS did under the first Trump administration, said Brian Blase, president of Paragon Health Institute and a healthcare policy adviser in the first Trump administration.
“They’ve hit the ground running and they had a plan and are executing on the plan,” Blase said in an interview. “Just in year-one accomplishments, they were able to get a lot more done in 2025 than we were able to get done in 2017.”
Pope helped the team of Trump administration CMS appointees before they assumed their roles to craft a range of reform initiatives “ready to roll out on day one.” That included shaping them to minimize the political and legal challenges they might face.
Many of those initiatives have already rolled out this year, he said.
Further policy changes are likely in Medicaid, technology-related policies and payments for Medicare Advantage plans.
Oz difference
The approach of Oz to leading CMS has been a marked departure from that of Seema Verma, the administrator of CMS under the first Trump administration, said Pope.
“He’s been bolder than Seema Verma was,” he said. “She was not as concerned with reining in the programs’ aggregate costs. She was actually onboard with a lot of CMMI [Center for Medicare and Medicaid Innovation] initiatives that had come out in the [ACA] and the Obama administration’s initiatives. She didn’t really push back on much of that.”
Verma, now an executive vice president and general manager, Oracle Health and Life Sciences, said that during her tenure with CMS, “I advanced innovation and fiscally conservative policies that saved taxpayer dollars and improved care quality for the American people. Any assertion to the contrary is absurd.”
“We took Medicare Advantage premiums to an all-time low, and through Patients over Paperwork, we saved 42 million hours of administrative work and approximately $6.6 billion between 2018 and 2021,” Verma said in an emailed response. “My site-neutral payment policy lowered copayments for beneficiaries and was estimated to drive more than $800 million in savings for the Medicare program and taxpayers in its first year.”
Other initiatives she cited included new kidney care models — estimated to generate savings of $23 million over 5 years — the first work requirement policy for Medicaid and an overhaul of the Medicare Shared Savings Program, which generated $1.19 billion in savings.
Oz’s skepticism of the Biden administration’s initiatives was seen in rolling back rules that would have grown both Medicaid state-directed payments and Medicare spending on social determinants of health, for example.
Oz’s role lobbying Congress on behalf of the recently enacted One Big Beautiful Bill Act (OBBBA) was widely described by lobbyists and policy watchers as significant for its passage. For example, Oz highlighted to skeptical Republicans the strong financial performance of some large not-for-profit health systems in order to downplay OBBA’s adverse financial effects on hospitals.
“He’s more hands on and a lot more visible, especially in a policy sense,” said Paulo Pontemayor, a lobbyist for the Catholic Health Association. “Really what we’ve seen in the last couple of months [is Oz] being deployed to the House and Senate to really explain components of the OBBBA. It [also] shows he has a big hands-on approach to its implementation.”
CMMI effect
The new CMS also has a markedly different view on the Center for Medicare and Medicaid Innovation (CMMI), Pope said.
The new leadership embodies “a strain of Republican thinking that looks at CMMI and is completely disenchanted with the idea that this is generating savings in any specific ways,” he said.
He said, the Obama administration used CMMI to grow spending. Illustrating possible spending concerns from the new CMS leadership was a Healthcare Leadership Council-funded examination of 18 CMMI models by Avalere Health that found some provided a total of $2.6 billion in Medicare savings while others increased total Medicare spending by $10.3 billion.
The ACA gave CMMI “a fair amount of statutory discretion” and the leadership has a desire to “really rein in what CMMI is doing,” he said
In March, CMMI announced plans to terminate four active models and cancel the development of two proposed models to focus on models for expansion based on projected savings and quality outcomes.
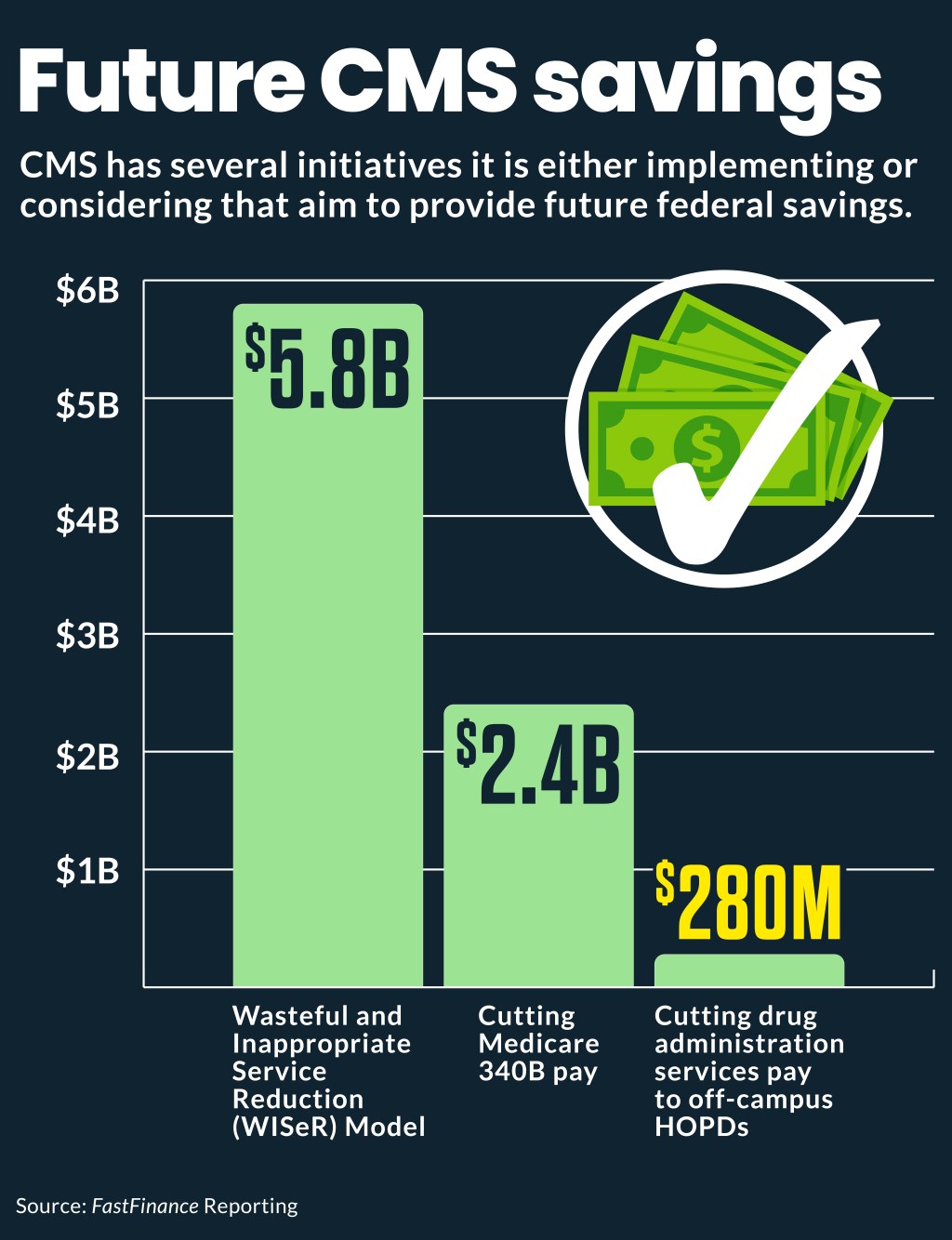
Recently announced from CMMI was the Wasteful and Inappropriate Service Reduction (WISeR) Model, to deploy AI and machine-learning technology as a tool to review services that are vulnerable to fraud, waste and abuse in traditional Medicare. The goal is to root out clinically unsupported care, on which Medicare spent $5.8 billion in 2022, using technology sponsored by private vendors.
Pope said statutory guardrails will likely limit the amount of spending that model will be able to cut.
Payment rules
New approaches by CMS include policy changes in various CMS payment rules.
For instance, Medicare’s 2026 proposed rule for hospital outpatient care, would accelerate — from 0.5% to 2% — a planned all-hospital annual cut related to 2022 remedy payments for 340B hospitals. That accelerated repayment would largely wipe out the planned 2026 rate increase for the 3,270 hospitals subject to it.
The proposed rule also included:
- A $280 million cut from paying drug administration services furnished in off-campus hospital outpatient departments (HOPDs) at the physician payment rate
- A notice of intent to conduct a survey to gauge hospitals’ acquisition costs for covered outpatient drugs — required before re-trying Medicare 340B drug pay cuts previously attempted in the first Trump administration
Benedic Ippolito, a senior fellow at the American Enterprise Institute, highlighted the site-neutral and 340B policies among initiatives of the new CMS leadership that he said were the most likely to upset hospitals.
Taken together, the many initiatives seem like a different, more hostile view of hospitals than that of the CMS leadership in previous administrations. “Especially on the administration side, if you add up everything,” Ippolito said.





