AI technology brings wholesale CDI benefits to Intermountain Health
Rather than eliminating jobs, a new tool the health system is using has made them more fulfilling.
At a time when the healthcare labor picture is marked by sustained high costs and shortages of key roles, one department at Intermountain Health found a way to operate as though it had six additional FTEs without an increase in the headcount.
The enhanced productivity was one benefit of implementing AI technology in clinical documentation improvement (CDI). The Salt Lake City-based, 33-hospital system also realized a financial ROI of 3-to-1 or better in the cases impacted by the tool, and it bolstered key care processes.

Such progress also manifested in employee satisfaction, which had been ebbing among some of the organization’s nurse CDI specialists.
Several specialists previously had communicated “that they would come in in the morning, they would look at their list and they would know that they didn’t have anything to offer in the work that they were going to do, which felt very discouraging as a clinician who previously was making such a big impact on people’s lives,” said Kearstin Jorgenson, operations director for physician advisor services with Intermountain.
“That was just a really poignant moment for me, thinking that these individuals are very talented, they’ve spent years at the bedside,” she said. “We’ve got to get them in a situation where they feel like they are contributing, where they’re engaged, they’re making a difference and making sure that that patient’s story is recorded accurately.”
Pinpointing a need
Intermountain rolled out a systemwide implementation process for the AI tool in phases, seeking to enhance CDI capabilities amid staffing constraints. The organization’s transition to a new benchmarking system had revealed gaps in key KPIs.

“We realized our national peers in the country were staffed almost four times as high as us,” said Sathya Vijayakumar, senior manager for clinical operations with Intermountain, noting the health system had roughly 0.25 FTEs per 1,000 charts, compared with somewhere around 0.99 for organizations like Mayo Clinic and Cleveland Clinic.
With respect to matching those systems’ quality and outcomes, Vijayakumar said, “There’s no way we’re able to compete at that level without getting some support [or] hiring more bodies. That’s why we chose the technology route.”

The goal was to create an infrastructure featuring integrated workflows in which CDI queries were conducted proactively.
“We had the traditional CDI folks who are scouring charts, and they’re sending queries to the providers to answer and get clarification,” said Kory Anderson, MD, assistant chief medical officer for clinical excellence with Intermountain. “The idea behind the AI piece was: Can we get upstream of the documentation with the provider so that as I’m doing [documentation] as a hospitalist, if there is a lack of specificity, or if there are labs that indicated a diagnosis I s a hospitalist, if there is a lack of specificity, or if there are labs that indicated a diagnosis I have not documented yet, .… the technology [can] maybe nudge me or prompt me to say, ‘Hey, is that something worth documenting if relevant and appropriate?’”
Engineering a better system
Working with its vendor partner, Intermountain implemented a tool that featured real-time documentation nudges to physicians during note writing. Test groups of physician advisors helped to refine the technology, which uses natural language understanding. The nudges, along with an evidence sheet, are accessible for review by CDI specialists.
A key expediting factor was the integration of the tool into clinicians’ workflows. The solution appears in a control bar alongside the electronic health record and acts as a single interface for all CDI-related insights. That integration ensures clinicians receive relevant, real-time feedback without a disruption in their documentation processes.
To prevent “nudge fatigue,” Intermountain Health rolled out the solution gradually over a year. Implementation was prioritized in areas with the highest potential impact, starting with frequently under-documented diagnoses such as heart failure. The team used benchmarking data to identify service lines with high potential for both financial and quality improvement, and then worked to develop customized, service-line-specific nudges.
Generating positive feedback
Along with boosts in revenue and productivity, Intermountain realized increases in case mix index and measures of illness severity and mortality risk, indicating conditions were being documented more comprehensively.
Nurses conducting CDI reviews were happy for the opportunity to focus on complex cases. With more than 210,000 inpatient admissions a year, Anderson said, “We do not have the staff to look at all of those accounts every day. We have to be very efficient in how we determine which cases to invest our time [in].”
“The AI really does some of the more straightforward [CDI] queries, but what we’ve seen an increase in is some of the more nuanced queries,” Jorgenson said. “I actually think there’s a direct correlation with caregiver engagement because our nurses are really being able to leverage that clinical knowledge and experience. They’re not just doing those head-slappers or easy conditions.”
Customization of AI triggers and queries ensured documentation was aligned with care goals. One specific nudge, which was created following a request from nephrologists at the health system, augmented nephrology consults and subsequent follow-up by improving documentation of acute kidney injury.
“It’s been a fantastic thing from the standpoint of having individuals actually soliciting help with our AI tools,” Jorgenson said. “You start to get a reputation that you have tools that can be helpful [and] that can make life easier for different clinicians as they’re trying to reach their goals.”
Smaller and rural facilities within the organization particularly benefited from the AI support.
“Using the tool allowed those physicians at those smaller facilities to still get some documentation improvement and impact, even though we as a CDI team just don’t have the bandwidth to regularly look at those accounts,” Anderson said.
Impact on charting efficiency
APP time and drive documentation excellence,” case study, Feb. 21, 2025
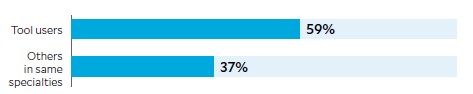
During a testing phase, physicians and advanced practice providers who
used the AI tool at Intermountain Health were more likely to complete
charting during or immediately after rounds.
Enhancing change management
Among veteran CDI specialists, there was some concern about whether their skill sets would be rendered redundant, Vijayakumar said. Newer members of the team tended to embrace the technology more quickly as a tool to help compensate for their inexperience.
Interaction with leadership is vital to ensure the productivity gains from such tools are not viewed as a reason to consider downsizing in the name of efficiency.
“You can easily go down that path [of workforce reductions] with leaders if you’re not consistently engaged with them — if you’re not keeping them in the loop about
what the numbers [are] and [what] the story really is that’s being crafted and told,” Anderson said.
One key was improved specificity in data analysis, allowing project leaders to report on what share of ROI continued to be from staff as opposed to directly from the tool.
“We could identify that AI is one of the legs of the stool and not the stool itself,” Vijayakumar said. “That helped convince our leaders that you can’t just take out [another stool] leg and reduce personnel, because they’re still bringing in value.”
The intensive compliance requirements around CDI automation tools mean even the most advanced technology is far from self-sufficient.
“If anything, we’re still making the case to try to hire more FTEs,” Anderson said.
Intermountain Health CDI initiative: By the numbers
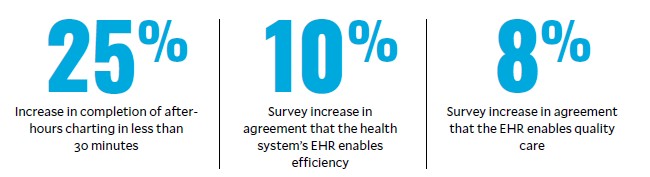
time and drive documentation excellence,” case study, Feb. 21, 2025
The impact of the AI tool implemented by Intermountain Health to enhance its clinical documentation
improvement program, relative to colleagues who were not using the tool.
Looking ahead
Intermountain hopes to use AI to expand the scope of its CDI initiatives. The idea is to impact not only documentation and payment, but even the quality of healthcare delivery. That potential already is seen in the tool’s ability to funnel documentation to case managers when chart terminology suggests the patient is nearing end of life and would benefit from conversations about goals of care and a potential transition to a hospice setting.
Enhanced CDI also can expedite processes involved in quite possibly the most vexing part of the healthcare revenue cycle.
“The biggest area of concern for most health systems is in the denials world,” Vijayakumar said. “There’s active work going on right now to automate some of the [utilization review] processes that our physician advisors work on, like your two-midnight reviews, your
inpatient-only criteria reviews. There’s a lot that can be automated and set up so you are not manually reviewing the chart and checking boxes.”
Where is the potential for AI next?
“I think anywhere you look where there’s a systematic process and people are manually checking boxes, you can have AI do that for you,” Vijayakumar said.
“That’s not to say there’s no need [for human resources], because at the end of the day, if those boxes are not checked, it is going to go to a physician, it is going to go to a nurse. but it’s going to optimize our process, and instead of looking at 25 charts, they’re probably going to look at 10 charts.”





